Workers Compensation Denials: Struggles Beyond the Injury
Every RCM director and coder familiar with Workers Compensation claims knows the feeling: a sinking sensation as another denial rolls in. Processing these claims can fill you with frustration. This blog will shed light on some of the most common struggles with Workers Comp claims and the denials they trigger.
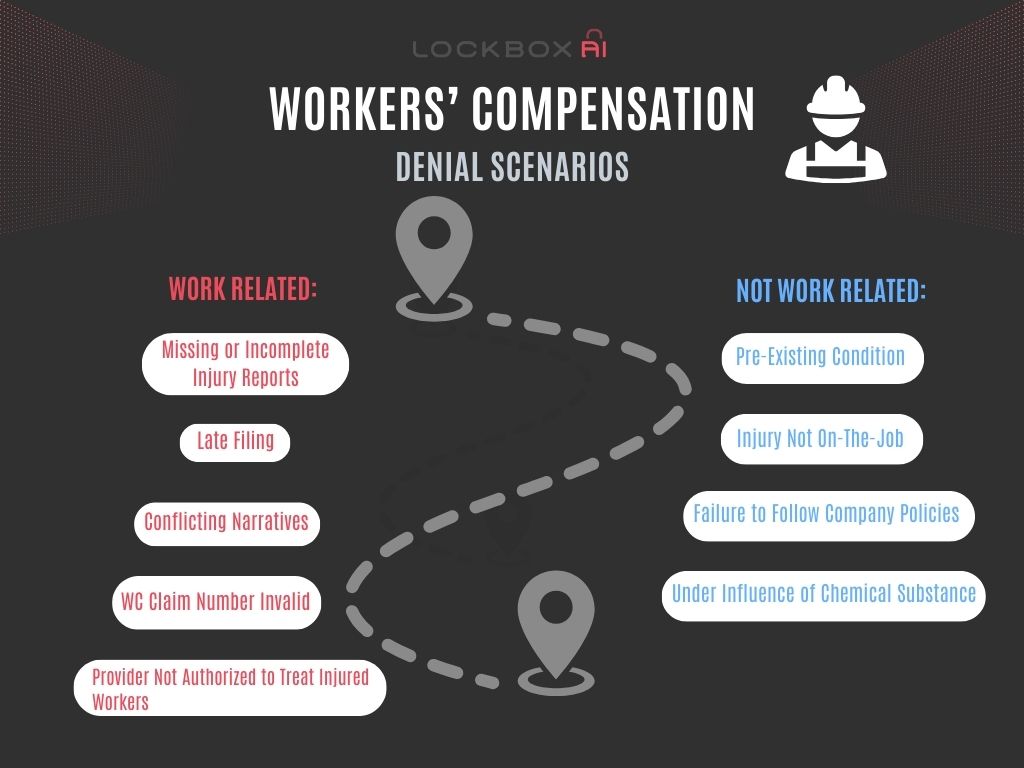
Here are just a few of the hurdles you might face when dealing with Workers Compensation claims:
- Missing or Incomplete Injury Reports: A critical piece of any Workers’ Comp claim is the initial injury report. Often, these reports are delayed or arrive incomplete, lacking crucial details about the accident, cause of injury, and how it relates to the job. Without this information, building a strong case becomes an uphill battle.
- Conflicting Narratives: Sometimes, the employee’s account of the injury might differ from the employer’s version of events. This discrepancy can make it difficult to determine if the injury truly qualifies for Workers Compensation benefits.
- Unclear Diagnoses: Vague or incomplete medical diagnoses can leave room for interpretation by the insurance carrier. This ambiguity might lead to denials based on the claim not meeting specific medical criteria for a work-related injury.
- Timely Reporting Issues: There are often strict deadlines for reporting work injuries. If the claim isn’t filed within the designated time frame, it could be automatically denied.
- Pre-Existing Conditions: If an employee has a pre-existing condition, the insurance carrier might argue that the work injury only aggravated a pre-existing problem, potentially leading to a denial of benefits.
Common Reasons Your Workers Compensation Claim Gets Rejected
Now, let’s delve into some of the most frequent reasons Workers’ Comp claims get denied:
- Injury Not Deemed Work-Related: If the insurer determines the injury didn’t occur on the job or wasn’t caused by work activities, the claim will likely be denied.
- Lack of Proper Documentation: Missing or incomplete paperwork, including medical records or witness statements, can be grounds for denial.
- Late Filing: As mentioned earlier, exceeding the deadline for reporting a work injury can lead to an automatic rejection.
- Questionable Cause: If the cause of the injury is unclear or there’s conflicting information, the insurer might deny the claim while they investigate further. Perfect examples are in the case of an employee’s failure to follow company procedures or the employee was known to be intoxicated or under the influence of a chemical substance. These things can raise doubts about the claim’s legitimacy.
Common Denial Phrases and Explanations:
- “Ongoing Responsibility for Medicals (ORM)”: This indicates a previous insurer is responsible for covering medical expenses related to a specific diagnosis, even if the injury occurred earlier.
- “Workers Compensation Claim Number Invalid”: Reasons include typos, outdated numbers, incorrect format, claim status changes, carrier/employer changes, fraudulent attempts, technical issues, or administrative errors.
- “Patient Must Use Workers’ Compensation Set-Aside (WCSA) Funds”: This means the requested service falls within your WCSA, and your claim is denied because those funds should be used first.
Stop the Denials: How to Streamline Your Workers Compensation Process
Feeling overwhelmed? Here are some tips to get your Workers’ Comp claims flowing smoothly and avoid denials:
- Develop a System for Injury Reporting: Encourage employees to report injuries immediately and have a clear, standardized process for collecting and documenting all relevant details.
- Accurate ICD10 Coding: Specific “Z” codes are used to link the injury to the workplace.
- Maintain Clear Communication: Open communication between employer, employee, and healthcare providers is crucial. Ensure everyone involved understands their role in documenting the injury and treatment plan.
- Stay on Top of Deadlines: Be aware of your state’s specific deadlines for reporting work injuries and filing claims. Don’t let time slip away and jeopardize the claim’s validity.
- Partner with a Reliable Medical Provider Network: Having a network of healthcare providers familiar with Workers Compensation procedures can ensure clear and timely diagnoses that support your claims.
By implementing these strategies, you can significantly reduce the number of denials you face and ensure your team can efficiently process legitimate Workers Compensation claims. Remember, a little preparation can save you a lot of frustration down the line!