Introduction
Electronic Health Record (EHR) systems revolutionize the way healthcare professionals manage patient information. Unlike traditional paper-based records, EHRs digitize medical data, providing quick access to comprehensive patient histories, medications, allergies, and test results.
Enhancing Efficiency and Accuracy in Healthcare Documentation
With EHR systems, physicians can efficiently document patient encounters in real-time, eliminating the need for manual charting. This not only saves time but also reduces the risk of errors commonly associated with handwritten notes.
- Real-Time Documentation: Physicians can document patient encounters directly into the EHR system during appointments, eliminating the need for manual charting.
- Templates and Smart Forms: EHRs offer customizable templates and smart forms that facilitate efficient documentation while ensuring standardization and compliance with clinical guidelines.
- Reduced Documentation Errors: With features such as auto-population of data and built-in error checks, EHR systems help minimize documentation errors, improving the accuracy of medical records.
- Time-Saving Benefits: The automation of documentation tasks frees up valuable time for healthcare providers, allowing them to focus more on patient care.
Streamlining Patient Care Delivery
EHR systems facilitate seamless collaboration among healthcare providers by enabling instant sharing of patient information. This streamlines the care delivery process, ensuring timely interventions and continuity of care.
- Interoperability: EHR systems facilitate the exchange of patient information among different healthcare settings, including hospitals, clinics, and pharmacies, promoting seamless care coordination.
- Care Plan Management: Healthcare teams can create and update care plans within the EHR system, ensuring that all providers are aligned with the patient’s treatment goals and preferences.
- Medication Management: EHRs include features for medication reconciliation, electronic prescribing, and alerts for drug interactions, enhancing medication safety and adherence.
- Remote Monitoring and Telehealth Integration: Some EHR systems support remote monitoring of patients’ health metrics and integration with telehealth platforms, enabling virtual consultations and remote patient monitoring.
Improving Communication and Coordination among Healthcare Providers
By centralizing patient data, EHR systems promote effective communication and coordination among various healthcare stakeholders, including physicians, nurses, and pharmacists. This interdisciplinary approach fosters better patient outcomes.
- Centralized Communication Hub: EHR systems serve as a centralized platform for exchanging messages, sharing updates, and collaborating on patient care plans among healthcare team members.
- Task Assignment and Tracking: Providers can assign tasks, set reminders, and track the progress of care activities within the EHR system, ensuring accountability and follow-up.
- Care Transitions: During transitions of care, such as hospital discharge or referral to a specialist, EHRs facilitate the transfer of relevant patient information, reducing the risk of gaps in care.
Impact on Physician-Patient Interactions
While EHR systems offer numerous benefits, some argue that excessive screen time during patient consultations may hinder the quality of physician-patient interactions. Striking a balance between technology use and interpersonal communication is crucial to maintaining patient trust and satisfaction.
- Balancing Technology Use: Physicians must strike a balance between using EHR systems to access patient information and maintaining meaningful face-to-face interactions with patients.
- Patient Education and Engagement: EHRs offer opportunities for patient education through the sharing of educational materials, lab results, and treatment plans, fostering patient engagement in their care.
- Addressing Patient Concerns: Healthcare providers should address any patient concerns or discomfort related to EHR use during appointments, ensuring that technology enhances rather than detracts from the patient experience.
Ensuring Data Security and Privacy
As healthcare data becomes increasingly digitized, safeguarding patient information against security breaches and unauthorized access is paramount. EHR systems employ robust security measures such as encryption and access controls to protect sensitive data.
- HIPAA Compliance: EHR systems must comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations to safeguard patient confidentiality and privacy.
- Encryption and Access Controls: EHRs employ encryption techniques and access controls to protect patient data from unauthorized access or breaches.
- Regular Security Audits: Healthcare organizations conduct regular security audits and risk assessments to identify vulnerabilities and ensure the integrity of their EHR systems.
- Employee Training: Staff members receive training on security best practices and protocols to prevent data breaches and mitigate potential risks to patient information.
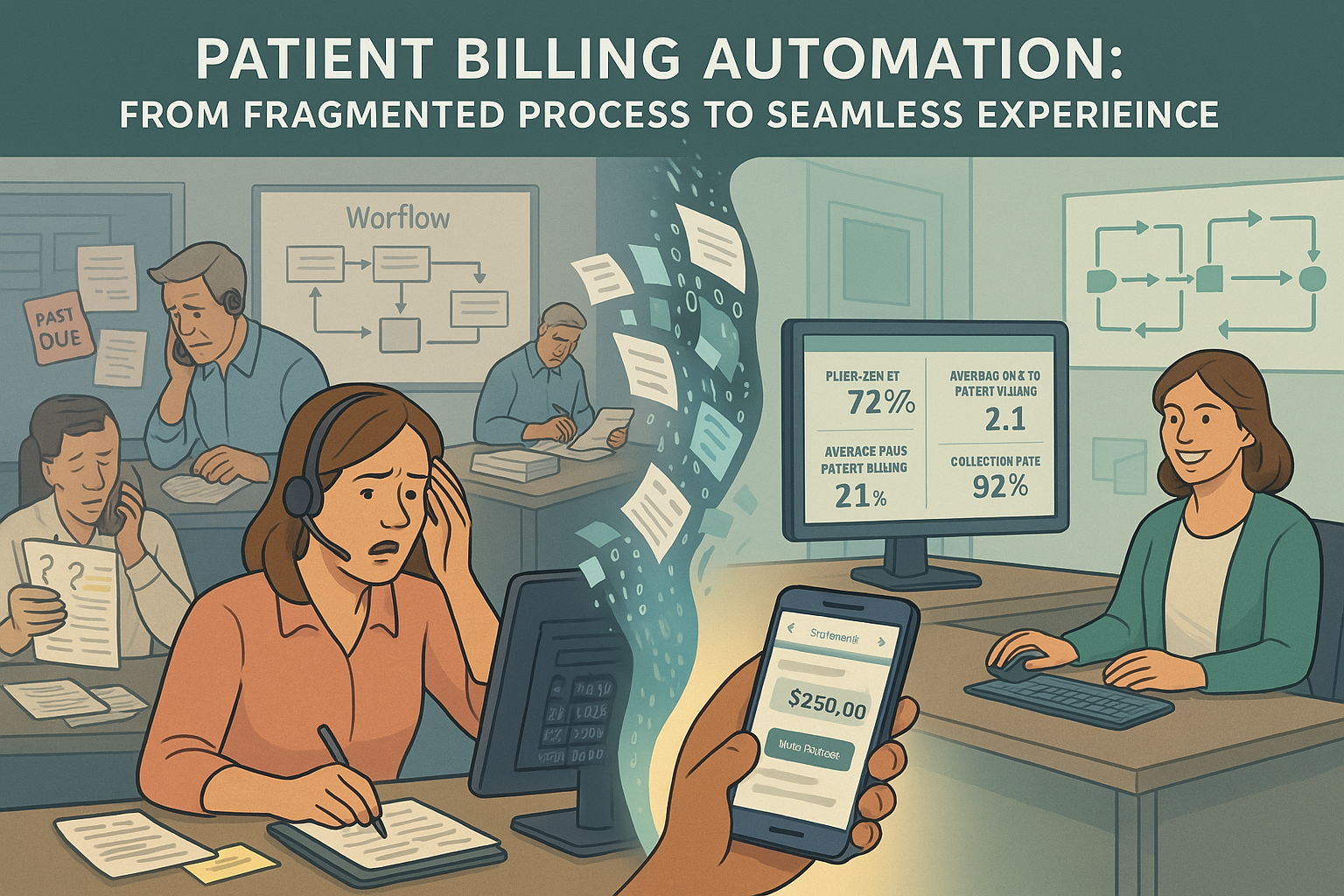
Integrating with Revenue Cycle Management
EHR systems play a vital role in revenue cycle management by capturing essential billing and coding information during patient encounters. This integration streamlines the billing process and enhances revenue capture for healthcare organizations.
- Capturing Billing Information: EHR systems capture essential billing information, such as procedure codes, diagnosis codes, and patient demographics, during the documentation process.
- Automated Charge Capture: Through automated charge capture functionalities, EHRs identify billable services rendered during patient encounters, reducing the risk of revenue leakage.
- Claims Submission: EHRs support electronic claims submission to payers, expediting the reimbursement process and reducing administrative overhead associated with paper claims.
- Revenue Cycle Analytics: Some EHR systems offer built-in analytics tools to track key performance indicators (KPIs) related to revenue cycle management, allowing organizations to identify trends and areas for improvement.
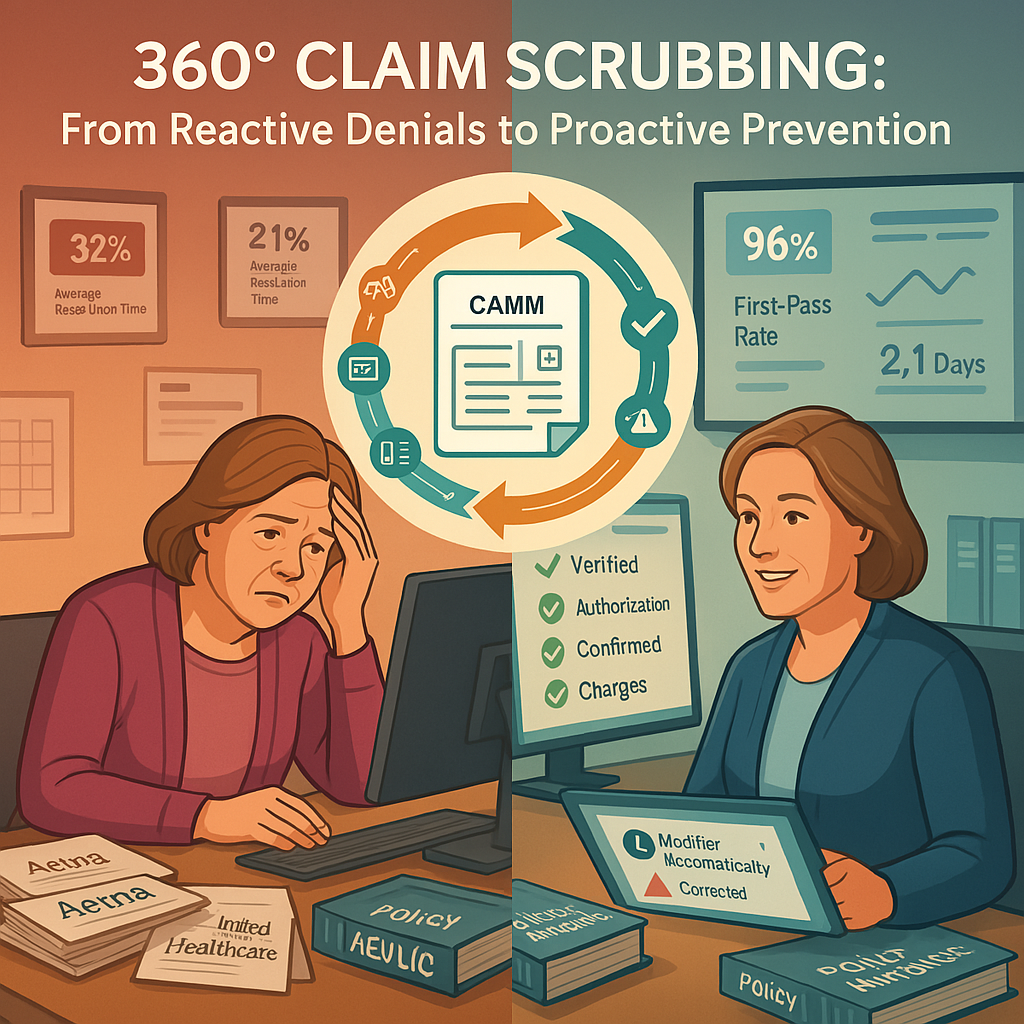
Optimizing Billing and Coding Processes
Through automated coding suggestions and electronic claims submission, EHR systems help healthcare providers optimize billing and coding processes, reducing the risk of billing errors and claim denials.
- Coding Assistance: EHR systems provide coding assistance through features such as code suggestions, guidelines, and built-in documentation templates, ensuring accurate code selection.
- Real-Time Edits and Alerts: EHRs flag potential coding errors or inconsistencies in real-time, enabling providers to address issues promptly before claims submission.
- Compliance Checks: Electronic Health Record systems incorporate compliance checks to ensure that billing practices align with regulatory requirements reducing the risk of claim denials.
- Streamlined Reimbursement: By automating billing and coding processes, EHRs streamline reimbursement workflows, leading to faster payment cycles and improved cash flow for healthcare organizations.
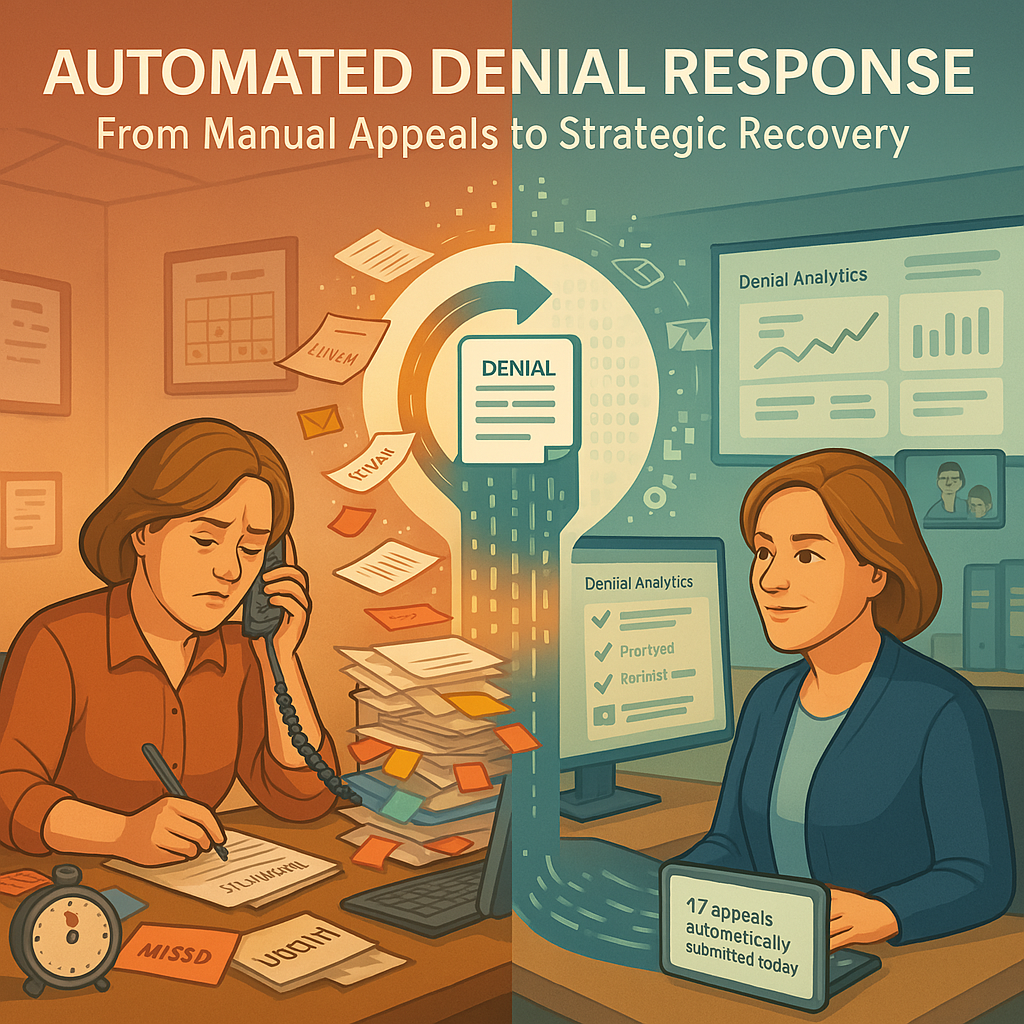
Minimizing Revenue Cycle Errors
By standardizing documentation practices and automating revenue cycle workflows, EHR systems minimize errors of coding discrepancies, claim submissions, thereby improving revenue cycle.
- Documentation Integrity: Electronic Health Record systems promote documentation integrity by capturing detailed and accurate patient data, reducing errors in billing.
- Claims Scrubbing: EHRs include claims scrubbing tools that check claims for errors before submission, minimizing the risk of claim rejections.
- Denial Management: Organizations use EHR data analytics to identify reasons for claim denials and implement strategies to reduce denial rates.
- Continuous Improvement: By leveraging data insights from Electronic Health Record systems, organizations can continuously refine their revenue cycle processes to optimize efficiency.
Enhancing Revenue Capture and Financial Performance
Efficient utilization of Electronic Health Record systems leads to improved revenue capture and enhanced financial performance for healthcare providers. By maximizing reimbursement opportunities and reducing administrative costs, organizations can achieve greater profitability.
- Maximising Reimbursement Opportunities: EHR systems help healthcare organizations maximize reimbursement opportunities by accurately documenting billable services.
- Reducing Revenue Leakage: Through improved coding accuracy, claims submission processes, and denial management strategies, EHRs minimize revenue leakage.
Challenges and Limitations of EHR Systems
Despite their benefits, Electronic Health Record systems come with their set of challenges, including usability issues, interoperability concerns, and data entry burdens. Addressing these challenges is crucial to realizing the full potential of EHR technology.
Future Trends and Innovations in EHR Technology
The future of EHR systems holds promising advancements, including artificial intelligence, machine learning, and predictive analytics. These innovations aim to further enhance clinical decision-making, personalise patient care, and optimise healthcare delivery.
Conclusion: Embracing the Evolution of Healthcare
In conclusion, EHR systems have transformed the landscape of healthcare delivery, offering numerous benefits for both physicians and patients. From streamlining documentation processes to optimising revenue cycle management, the impact of EHR systems is undeniable. As technology continues to evolve, embracing these advancements is crucial for delivering high-quality, patient-centered care in the digital age.