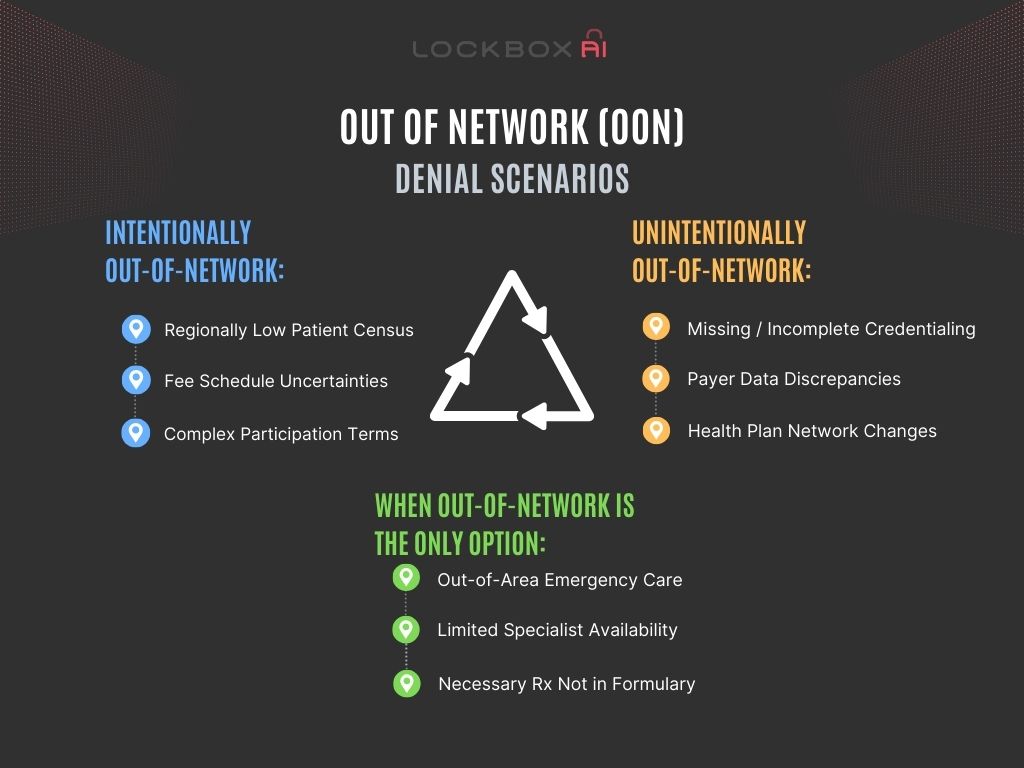
Understanding the Complexity of OON Claim Denials
OON claim denials occur when a patient receives medical services from a provider that is not contracted with their insurance company. Despite being insured, patients may find themselves facing hefty bills if their insurer refuses to cover the costs, citing the services as out-of-network denial.
Let’s face it, folks. As a claim denial manager, you get frustrated when claims get denied because a provider is listed as out-of-network. You’re either IN or you’re Out – right? Let’s drill into why it is not always so straightforward.
The Intentional Out-of-Network Denial:
The financial repercussions of OON claim denials can be significant. Patients may be responsible for paying the full cost of services received, which often exceeds what they would have paid for in-network care. This unexpected financial burden can lead to stress, debt, and even bankruptcy for some individuals and families. Sometimes, a provider or organization chooses to be out-of-network for a specific health plan. This can happen for a few reasons:
- Contract Disagreements: Maybe the health plan’s contract terms aren’t favorable for the provider, with low reimbursement rates or strict rules. In this case, the provider might prefer to see patients on a self-pay basis or accept other insurance plans.
The Unintentional Out-of-Network:
But not all out-of-network claims are intentional. Here’s where things get tricky:
- Credentialing Chaos: Credentialing issues can lead to denials even if a provider intends to be in-network. Missing information, delays in processing, or errors in the health plan’s system can leave a provider listed incorrectly.
- Data Discrepancies: Sometimes, there are simple mismatches between how a provider’s information is listed in our system and how it appears in the health plan’s database. A typo in a name or address can be enough to trigger an out-of-network denial.
- Plan Changes and Time Lag: Health plans update their provider networks regularly. There might be a lag between a provider joining a network and the information being reflected in the plan’s system, leading to a temporary out-of-network status.
When Out-of-Network is the Only Option:
Of course, there are situations where going out-of-network is unavoidable:
- Emergency Care: If you need urgent medical attention and can’t reach an in-network provider, you likely qualify for out-of-network denial coverage under most health plans.
- Specialist Availability for Out-of-Network Denial: Sometimes, a specific specialist you need might not be in-network with your plan. This might be a valid reason to seek out-of-network care, but be sure to check your plan’s out-of-network benefits and potential costs beforehand.
- The Necessary Rx: No other IN-formulary drug for a specific condition are effective or available.
Fighting the Out-of-Network Denial:
If you believe an out-of-network denial is incorrect, here’s what you can do:
- Contact the Health Plan for out-of-network denial: The EOB will explain the denial reason. Look for details related to the provider’s network status which may need correcting.
- Contact the Credentialing Department: Verify if that provider’s credentials need updating.
- Appeal the Denial: If you have a valid reason for going out-of-network, work with your provider to submit an appeal to your health plan. Include any documentation supporting your case.
Navigating the Fine Print: Tips for Avoiding Out-of-Network Denial
To minimize the risk of OON claim denials, patients should familiarize themselves with their insurance plan’s network requirements. Before seeking medical treatment, it is crucial to verify that the provider is in-network and that the services are covered by the insurance plan. Additionally, obtaining pre-authorization for procedures can help prevent claim denials later on.
Conclusion
OON claim denials pose significant challenges for patients, often resulting in unexpected financial burdens and barriers to healthcare access. By understanding the complexities of insurance networks, advocating for legislative reforms, and proactively seeking in-network care, patients can mitigate the risks associated with OON claim denials and protect their financial health.
Thus by understanding the different scenarios – intentional out-of-network choices, unintentional network discrepancies, and true out-of-network denial needs – every department plays a role in staying current with providers’ network statuses.