Global Period Denials: Seemingly Simple Claims Getting Rejected
Every RCM director and coder has been there: a seemingly endless stream of denied claims. One of the most common reasons for these denials involves services included within a global period.
This blog will break down the world of global periods in healthcare claims. We’ll explore the types of services typically bundled into them, along with common denial scenarios. More importantly, we’ll show you when and how to fight back against global period denials.
What are Global Periods and Why Do They Cause Denials?
A global period refers to a specific time frame following a surgical or other medical procedure. During this period, the payment for the main procedure is considered to include certain related services. These might include follow-up visits, anesthesia, and some lab tests.
Here’s where things can get tricky. If a provider bills for an additional service performed within the global period, the claim might be denied. The payer sees it as double-billing since the initial payment already covered those services.
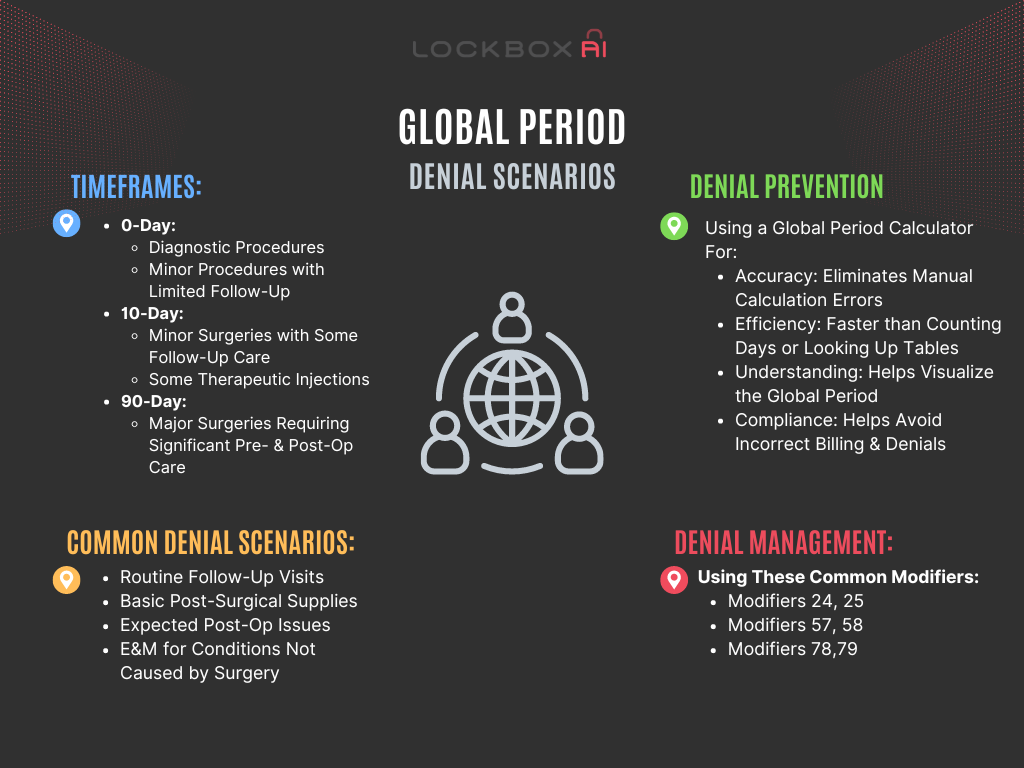
Here are some common denial scenarios related to global periods:
- Billing for a follow-up visit: If a routine postoperative visit falls within the global period for the surgery, a separate claim for that visit will likely be rejected.
- Billing for anesthesia: Similar to follow-up visits, if anesthesia is considered part of the global package for a procedure, a separate charge will be denied.
- Billing for additional tests: Some lab tests or X-rays might be bundled into the global fee, leading to denials for separate charges during the global period.
There are three main timeframes of global periods:
- 0-Day: This covers only the day of the procedure itself. Think of minor surgeries or endoscopies.
- 10-Day: The most common type covers the surgery and follow-up care for 10 days after.
- 90-Day: For more complex procedures covers the surgery and follow-up care for 90 days after.
Fighting Back: When Can You Appeal a Global Period Denial?
Not all global period denials are set in stone. Here are some situations where you might have a case for an appeal:
- Unforeseen complications: If a serious complication arises after the initial procedure, necessitating additional services beyond what’s typically included, this could be grounds for a successful appeal.
- Documentation errors: Double-check your coding and documentation. If there’s a clear error that justifies the additional service, appealing the denial might be worthwhile. Missing modifiers is a top reason to do a corrected claim such as when more complex dressing change is needed due to a wound complication.
- Pre-operative services: If medically necessary services were provided before the surgery but billed separately, they might not be considered part of the global period, allowing for a possible appeal. An example of this may be when An independent Medical Evaluation (IME) is performed by a separate physician before surgery to assess a patient’s medical fitness for the procedure.
Common Modifiers for Appropriate Use to Overcome Global Period Denials:
- Modifier 24: Unrelated evaluation and management service by the same physician during a postoperative period.
- Modifier 25: Significant, separately identifiable evaluation and management service by the same physician on the same day of the procedure or other service.
- Modifier 57: Decision for surgery.
- Modifier 58: Staged or related procedure or service by the same physician during the postoperative period.
- Modifier 78: Unplanned return to the operating room for a related procedure during the postoperative period.
- Modifier 79: Unrelated procedure or service by the same physician during the postoperative period.
Prevention is Key: Using a Global Period Calculator
A global period calculator tool can help prevent claim denials caused by erroneous billing for services included within a procedure’s global period.
The benefits of using a payor-provided calculator are the following:
- Accuracy: Calculators eliminate manual calculation errors, ensuring you know the precise end of the global period.
- Efficiency: It’s much faster than manually counting days or looking up tables, saving time for healthcare providers and billing departments.
- Understanding: The calculator helps visualize the global period, making it clearer what services are included or excluded within that time frame.
- Compliance: Knowing the correct global period helps avoid incorrect billing and potential denials.
Important Tip: Always check with the specific payer’s guidelines regarding global periods for the procedure at hand. Different payers might have slightly different policies.
Global periods are one of the more clearly defined areas of coding and billing. It is a highly preventable denial category. Identify a pattern to which services are most often the target of global period nonpayment and get to the root payer, provider, or team member that is triggering this repetitive denial. Feel the satisfaction of seeing the denials diminish!
Addressing global period denials requires a proactive approach from healthcare providers, including ongoing education and training for staff involved in coding and billing processes. Implementing robust documentation practices, conducting regular claim audits, and staying updated on changes to billing regulations and insurance policies can help mitigate the risk of denials.
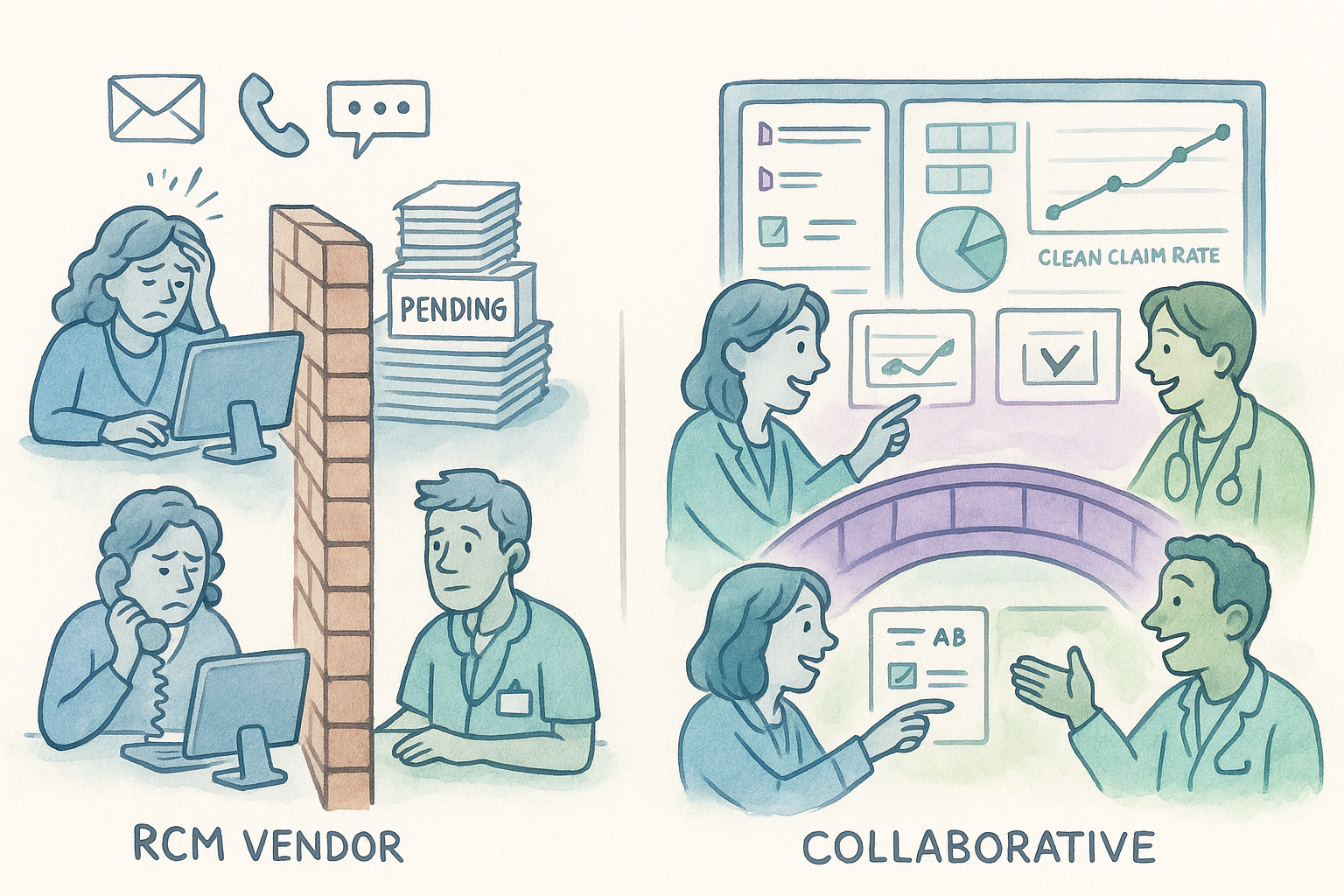
Furthermore, fostering open communication with payers and establishing protocols for addressing claim disputes can facilitate resolution in cases of denial. Collaboration between healthcare providers and insurers is essential for streamlining the claims process and ensuring timely reimbursement for services rendered.
Conclusion
Global period denials pose a significant challenge for healthcare providers, despite the apparent simplicity of claims falling within this timeframe. By identifying common causes of denials and implementing strategies to address them, providers can minimize revenue loss and enhance the efficiency of their billing operations. Effective communication, meticulous documentation, and adherence to coding and billing guidelines are essential for navigating the complexities of global period reimbursement.