In the realm of healthcare administration, one of the most challenging aspects for providers and patients alike is navigating the labyrinth of benefits denials. Understanding the reasons behind these denials is crucial for both improving the claims process and ensuring that patients receive the care they need. Central to this understanding are the Claim Adjustment Reason Codes (CARCs) and Remittance Advice Remark Codes (RARCs), collectively known as CARC/RARC descriptions, which provide standardized explanations for why claims are denied or adjusted. This article delves into the benefits of denials, focusing on the compilation and interpretation of CARC/RARC descriptions.
You’ve tackled a variety of benefits-related denials as covered in previous blogs. Here, we look at a compilation of those individual blogs as it is defined by CARC/RARC code sets.
What are CARC/RARC Descriptions?
CARC/RARC descriptions are codes used by insurers to communicate the status of a claim to healthcare providers. CARCs explain why a claim was paid differently than expected, either partially or not at all. These codes cover a wide range of reasons, including issues with patient eligibility, service coverage, or documentation requirements. RARCs, on the other hand, provide additional details or clarification about the CARCs, offering more specific information on the denial or adjustment.
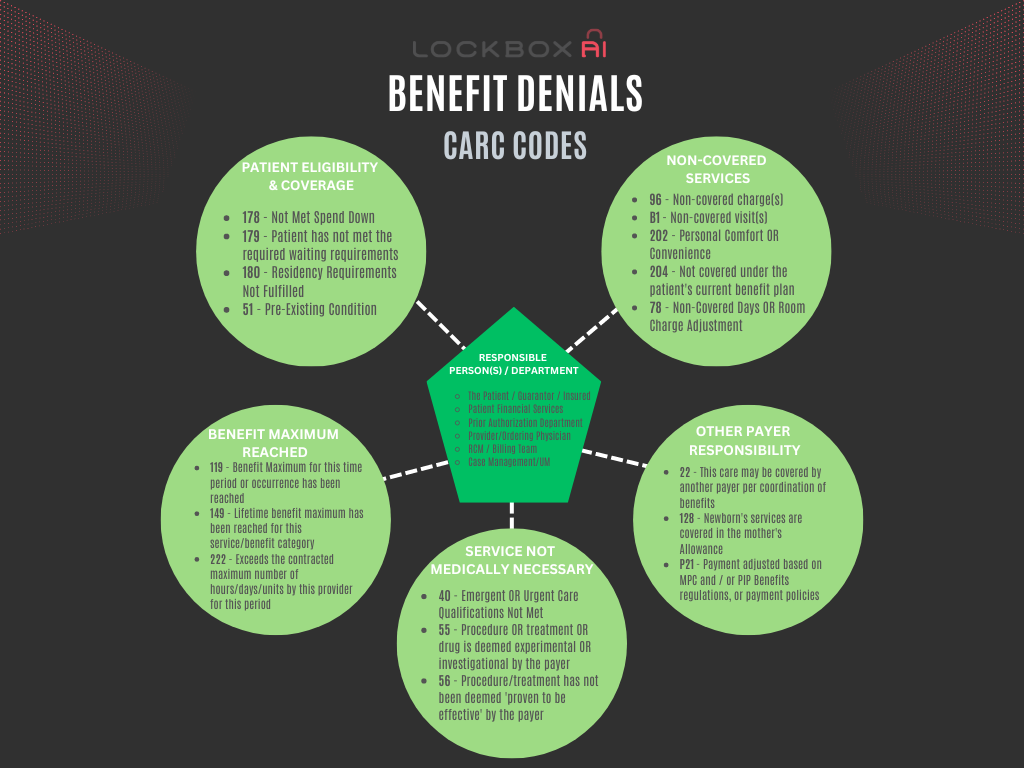
Here’s a breakdown of some common denial descriptions you might encounter:
- Patient Eligibility:
- Not Met Spend Down: The patient hasn’t met the financial requirements to access certain benefits.
- Waiting Period Not Completed: The patient hasn’t been enrolled in the plan long enough for specific services.
- Residency Requirements Not Fulfilled: The patient doesn’t reside in the required area for coverage.
- Non-Covered Services:
- Personal Comfort/Convenience: Services deemed unnecessary for medical treatment, like basic amenities.
- Not Covered by Benefit Plan: The specific service, equipment, or medication isn’t included in the patient’s plan.
- Non-Covered Days/Room Charge Adjustment: Limits on covered hospital days or specific room types have been exceeded.
- Benefit Maximum Reached:
- Benefit Maximum Reached: The patient has exhausted their lifetime or annual coverage limit for a particular service.
- Benefit Maximum for this time period or occurrence has been reached: The plan limits reimbursement for a specific condition or time period and that limit has been reached.
- Service Not Medically Necessary:
- Emergent/Urgent Care Qualifications Not Met: The service doesn’t qualify for the higher reimbursement rate associated with urgent care.
- Procedure/treatment/drug is deemed experimental/investigational by the payer: The plan does not cover services deemed experimental by their standards.
- Pre-Existing Condition:
- The plan excludes coverage for the specific pre-existing condition the service relates to.
- Other Payer Responsibility:
-
- This care may be covered by another payer per coordination of benefits.
- Another insurance plan may be the primary payer for this service.
- Newborn’s services are covered in the mother’s Allowance. Newborn care is often bundled within the mother’s coverage.
- Payment adjusted based on the Medical Payments Coverage (MPC) and/or Personal Injury Protection (PIP) Benefits jurisdictional regulations, or payment policies. Regulations for car insurance or related policies might reduce the healthcare plan’s payment responsibility.
The Importance of Understanding CARC/RARC Descriptions
- Improved Revenue Cycle Management: For healthcare providers, understanding CARC/RARC descriptions is vital for effective revenue cycle management. By accurately interpreting CARCs and RARCs, providers can address issues more swiftly and reduce the frequency of denied claims. This proactive approach can lead to quicker reimbursements and improved cash flow.
- Enhanced Patient Communication: Patients often find the claims process confusing and frustrating. By understanding CARC/RARC descriptions, providers can offer clearer explanations to patients about why a claim was denied and what steps can be taken to resolve the issue. This transparency can enhance patient trust and satisfaction.
- Targeted Staff Training: Healthcare facilities can use CARC/RARC descriptions to identify common issues and provide targeted training to their billing and coding staff. For instance, if a particular code frequently appears due to incorrect documentation, staff can be trained to ensure proper documentation practices are followed.
- Compliance and Risk Management: Accurate interpretation of CARC/RARC descriptions helps ensure compliance with insurance and regulatory requirements. It also aids in identifying and mitigating potential risks associated with improper billing practices, which could lead to audits or penalties.
Common CARC/RARC Descriptions
Here are some frequently encountered CARC/RARC descriptions:
- CARC 29: “The time limit for filing has expired.” This code indicates that the claim was submitted after the deadline set by the insurer.
- CARC 96: “Non-covered charge(s).” This suggests that the services provided are not covered under the patient’s insurance plan.
- CARC 197: “Precertification/authorization/notification absent.” This code points to the need for prior authorization for the service rendered, which was not obtained.
- RARC N30: “Patient ineligible for this service.” This remark provides additional details that the patient’s insurance does not cover the service in question.
- RARC MA130: “Your claim contains incomplete and/or invalid information, and no appeal rights are afforded because the claim is unprocessable.” This remark specifies that the claim cannot be processed due to missing or incorrect information.
Strategies for Managing Denials
- Regular Audits: Conduct regular audits of denied claims to identify patterns and areas for improvement. This can help in understanding the root causes of denials and taking corrective actions.
- Timely Appeals: Develop a systematic approach for appealing denied claims. Ensure that all necessary documentation and information are provided to support the appeal.
- Patient Eligibility Verification: Implement robust processes for verifying patient eligibility and benefits before services are rendered. This can prevent denials related to ineligibility or non-coverage.
- Prior Authorization: Ensure that prior authorizations are obtained when required. Maintain a checklist of services that typically require authorization and verify with insurers as needed.
- Clear Documentation: Maintain thorough and accurate documentation for all services rendered. Ensure that the documentation meets the specific requirements of different insurers.
It is no doubt that many of you have memorized the actual CARC and RARC code sets to the variations of benefits denials listed. Because many of these denials are complex enough to warrant their own discussions, we’ve dedicated individual blogs to explore them in depth. We hope you’ll refer to these resources (if you haven’t already) for additional insights.
Conclusion
Understanding the nuances of CARC/RARC descriptions is indispensable for healthcare providers aiming to minimize claim denials and optimize their revenue cycle. By leveraging these codes effectively, providers can enhance operational efficiency, ensure compliance, and improve patient satisfaction. Regular training and process improvements, coupled with a thorough understanding of denial reasons, can significantly reduce the occurrence of denials and lead to a more streamlined claims process.