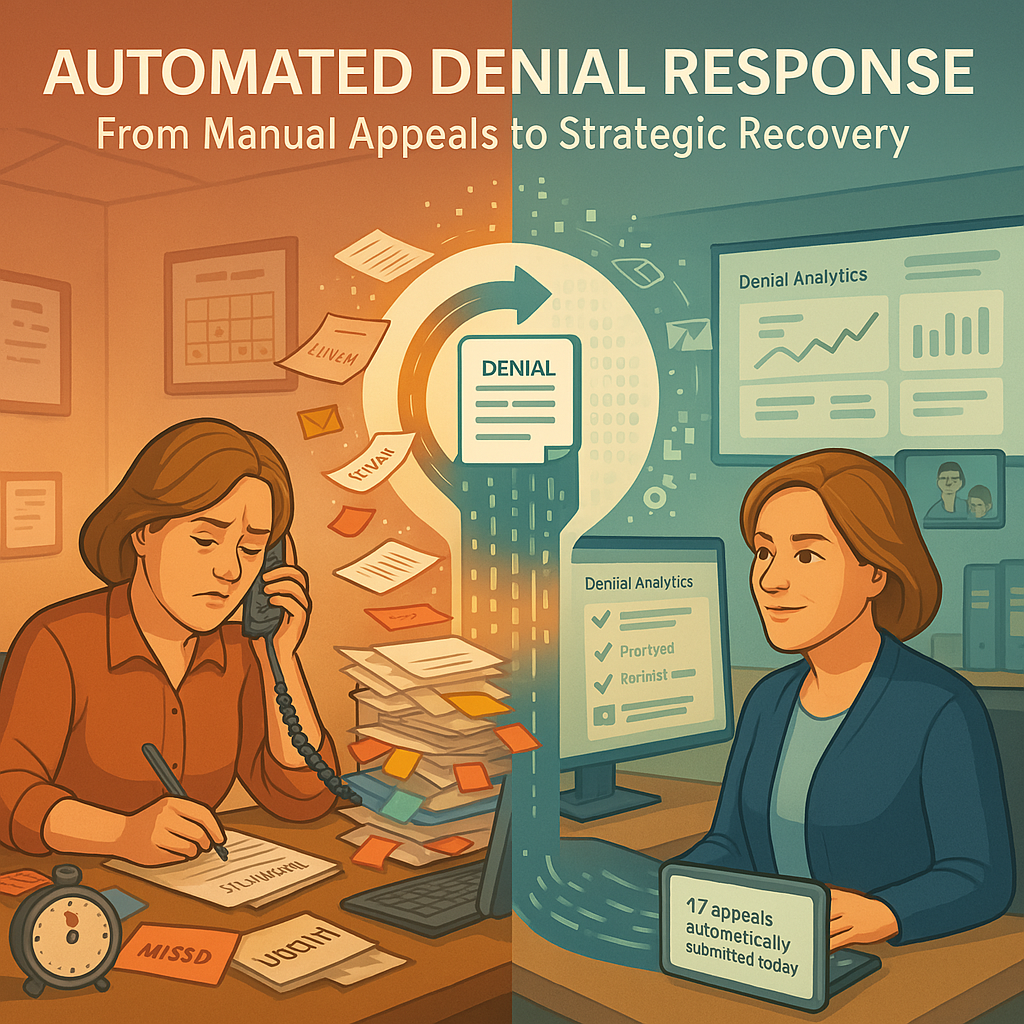
Despite the best prevention efforts, denials remain an unavoidable reality in healthcare revenue cycle management. While proactive measures can significantly reduce denial volume, the increasing complexity of payer requirements ensures that some portion of claims will continue to be denied—requiring efficient, effective response mechanisms to protect revenue.
The Costly Reality of Manual Denial Management
For most revenue cycle operations, the current denial management workflow creates significant operational challenges:
- Resource-intensive triage: The painstaking process of manually reviewing denial codes, determining appropriate actions, and routing to the right teams consumes hours of skilled staff time. The frustration of watching denial work queues grow while staff struggle to prioritize which accounts to work first creates both operational inefficiency and employee burnout.
- Incomplete context for appeals: Staff often lack easy access to the complete documentation needed to create effective appeals. The exasperation of having to search multiple systems to gather supporting information—knowing that any missed element could result in a failed appeal—creates unnecessary stress and delays in the response process.
- Inconsistent response quality: Appeal effectiveness varies widely based on staff experience and workload. The disappointment of discovering that appeals are being denied because they lack critical elements or contain inconsistent rationales represents one of the most avoidable sources of lost revenue in the denial management process.
- Missed appeal deadlines: The time-consuming nature of manual appeal preparation leads to missed filing deadlines. The particular frustration of identifying legitimate appeal opportunities only to discover the filing window has closed represents one of the most disheartening aspects of revenue cycle management.
- Limited performance visibility: Traditional denial management provides limited insight into appeal success rates by denial type and payer. The inability to systematically track which appeal strategies work—and which don’t—perpetuates a cycle of inefficiency that prevents continuous improvement.
These challenges don’t just impact financial performance—they create ongoing operational friction that demoralizes staff and limits the effectiveness of your entire revenue cycle operation.
Building on Foundation: The Integrated Automation Approach
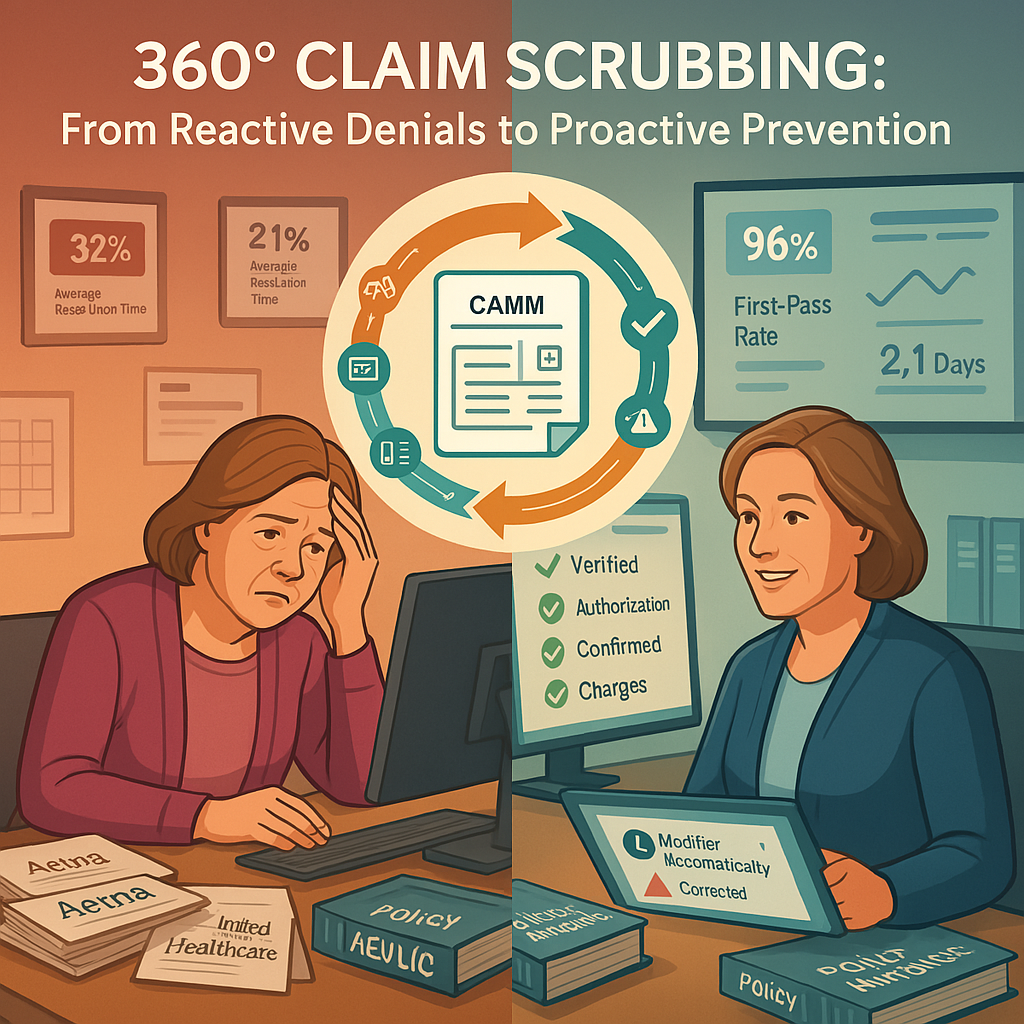
The Automated Denial Response solution builds directly on the foundation established by the first two components of our automation roadmap:
- Payment posting automation provides accurate, timely denial identification and classification
- 360-degree claim scrubbing prevents avoidable denials from occurring
- Automated denial response now ensures optimal handling of remaining denials
This integrated approach ensures that each component enhances the effectiveness of the others, creating a continuously improving revenue cycle ecosystem.
The Automated Denial Response Framework
Our comprehensive denial management solution transforms the appeal process through a multi-layered approach:
1. Intelligent Denial Triage and Routing
The system automatically:
- Analyzes denial codes against historical patterns
- Determines appropriate response strategies for each denial
- Routes denials to the optimal workflow or staff member
- Prioritizes work based on appeal deadlines and recovery potential
The relief of eliminating manual triage cannot be overstated. No more tedious sorting through work queues or attempting to decipher cryptic denial codes—the system instantly identifies the next best action and ensures denials reach the right resource at the right time.
2. Contextual Documentation Assembly
For each denial, the system:
- Gathers relevant clinical documentation from integrated systems
- Compiles previous claim and payment history
- Identifies payer-specific requirements for successful appeals
- Presents all necessary context in a unified workspace
The persistent struggle to assemble complete appeal documentation is eliminated. Staff no longer waste precious time hunting through multiple systems to gather supporting information—everything needed for effective appeals is automatically assembled and presented in a usable format.
3. Automated Response Templates
Based on denial type and payer, the system provides:
- Pre-populated appeal letters customized to specific denials
- Supporting regulation and policy citations relevant to the case
- Data-driven appeal narratives based on successful precedents
- Payer-specific formatting to meet submission requirements
The frustration of crafting appeals from scratch for each denial disappears. Staff leverage proven, effective templates that incorporate the exact elements needed for successful appeals—dramatically improving consistency and effectiveness while reducing preparation time.
4. Direct Response Channel Automation
For appropriate denial types, the system can:
- Submit appeals directly through payer portals
- Transmit medical records electronically
- Track submission status and confirmation numbers
- Monitor response timeframes to ensure timely follow-up
The tedious process of manually uploading documents to payer portals or preparing paper submissions is largely eliminated. Appeals reach payers faster, with confirmation tracking that prevents submissions from falling through the cracks.
Human-in-the-Loop Optimization
While automation drives efficiency, the system maintains critical human oversight:
Expert Review for Complex Cases
For denials requiring clinical judgment or policy interpretation, the system:
- Flags cases requiring human expertise
- Provides suggested approaches based on similar successful appeals
- Offers easy access to supporting documentation
- Learns from human decisions to improve future recommendations
This collaborative approach ensures that complex cases receive appropriate attention while still benefiting from automation support. The constant challenge of balancing thoroughness with productivity is addressed through intelligent workflow design that optimizes human intervention.
Continuous Learning from Outcomes
Unlike static denial management approaches, the system:
- Tracks appeal outcomes by denial type, payer, and strategy
- Identifies which appeal approaches are most effective
- Adjusts response templates based on success rates
- Refines triage logic based on recovery patterns
The perpetual challenge of determining which appeal strategies actually work is resolved through systematic tracking and analysis. Revenue cycle leaders gain unprecedented visibility into denial patterns and effective response strategies—creating a continuous improvement cycle that steadily increases recovery rates.
Beyond Traditional Appeals: Proactive Intervention
The system extends beyond traditional appeal workflows to include:
Medical Necessity Documentation Enhancement
For clinically-driven denials, the system:
- Identifies documentation gaps in clinical records
- Suggests specific documentation elements needed for successful appeals
- Facilitates efficient physician queries for additional information
- Compiles comprehensive clinical evidence to support medical necessity
The frustrating process of trying to construct medical necessity appeals without adequate clinical documentation is transformed. The system proactively identifies documentation needs and facilitates efficient collection of supporting information—dramatically improving success rates for clinical appeals.
Payer Behavior Analysis
Through continuous monitoring, the system:
- Identifies patterns in payer denial behavior
- Detects emerging denial trends before they become widespread
- Alerts to policy changes based on denial pattern shifts
- Recommends preventive measures to address new denial risks
The chronic struggle to stay ahead of changing payer practices becomes manageable. Revenue cycle leaders receive early warning of emerging denial trends—enabling proactive intervention before new denial patterns significantly impact revenue.
Implementation Considerations
For experienced revenue cycle leaders evaluating this solution, key considerations include:
- Integration breadth: Determining which clinical and financial systems to connect
- Appeal template customization: Balancing standard approaches with organization-specific elements
- Automation threshold settings: Configuring which denials can be fully automated versus requiring review
- Performance baseline measurement: Establishing current appeal success rates by denial type
- Staff transition planning: Preparing denial management teams for enhanced roles
Most organizations implement automated denial response in phases, beginning with high-volume, straightforward denial types and extending to more complex scenarios as confidence in the system grows. Full implementation typically requires 60-90 days, with measurable improvements in appeal volume and effectiveness visible within the first 30 days.
Performance Metrics and ROI
Organizations implementing automated denial response typically experience:
- 40-50% reduction in denial management labor costs
- 15-20% improvement in appeal success rates
- 30-40% faster appeal submission timeframes
- 10-15% increase in overall denial recovery
- 25-30% reduction in aged denials beyond appeal deadlines
These improvements create both immediate operational benefits through reduced labor costs and substantial financial gains through improved recovery rates and accelerated cash flow.
The Complete Revenue Cycle Automation Picture
With automated denial response, the third component of our automation roadmap is now in place:
- Payment posting automation ensures accurate, timely posting and denial identification
- 360-degree claim scrubbing prevents avoidable denials from occurring
- Automated denial response maximizes recovery for unavoidable denials
Together, these three components create a comprehensive approach to revenue cycle automation that addresses the entire denial lifecycle—from prevention through recovery.
Conclusion
By implementing automated denial response, revenue cycle operations transform one of their most labor-intensive processes into a streamlined, data-driven workflow that maximizes recovery while minimizing staff burden. Rather than struggling to keep pace with denial volume, organizations can systematically analyze denial patterns, implement targeted prevention strategies, and optimize recovery efforts for unavoidable denials.
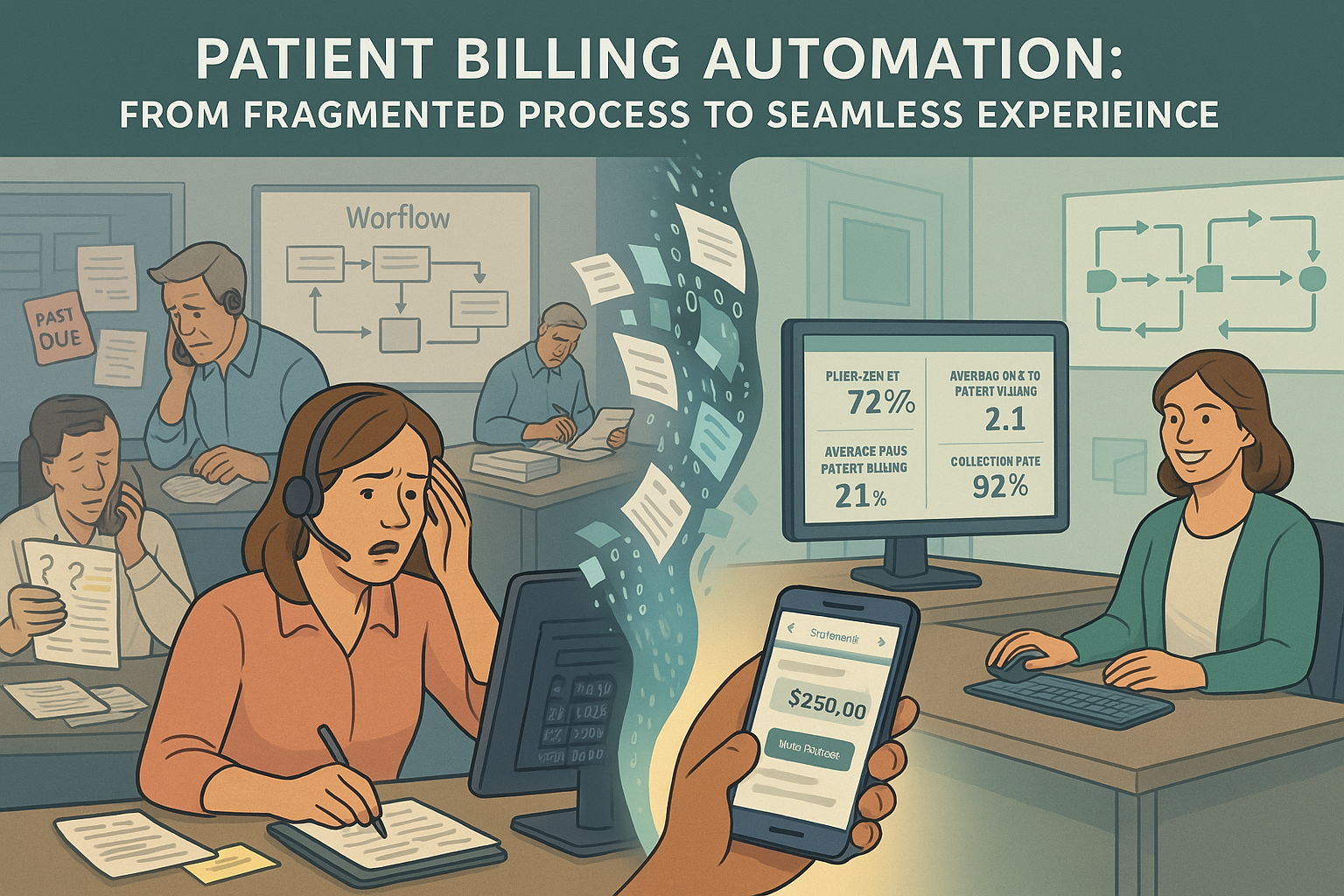
In our next article, we’ll explore how these foundational components enable the fourth element of our automation roadmap: patient billing automation to optimize the patient financial experience.