Elevating RCM Outcomes: Precision Tactics for Denial Resolution
Revenue Cycle Management (RCM) continues to evolve, facing new challenges such as effective denial management and enhancing team collaboration. Among the myriad challenges in RCM, managing claim denials stands out as a significant hurdle. Denial management, the process of identifying, analyzing, and resolving rejected claims, can drastically impact a healthcare provider’s revenue stream. Personalizing denial management techniques has emerged as a sophisticated approach to enhancing RCM outcomes. By leveraging precision tactics tailored to the unique characteristics of each claim and patient interaction, healthcare organizations can improve their financial health and ensure better patient care. Here’s a strategic approach to refining RCM operations.
Understanding Denial Management
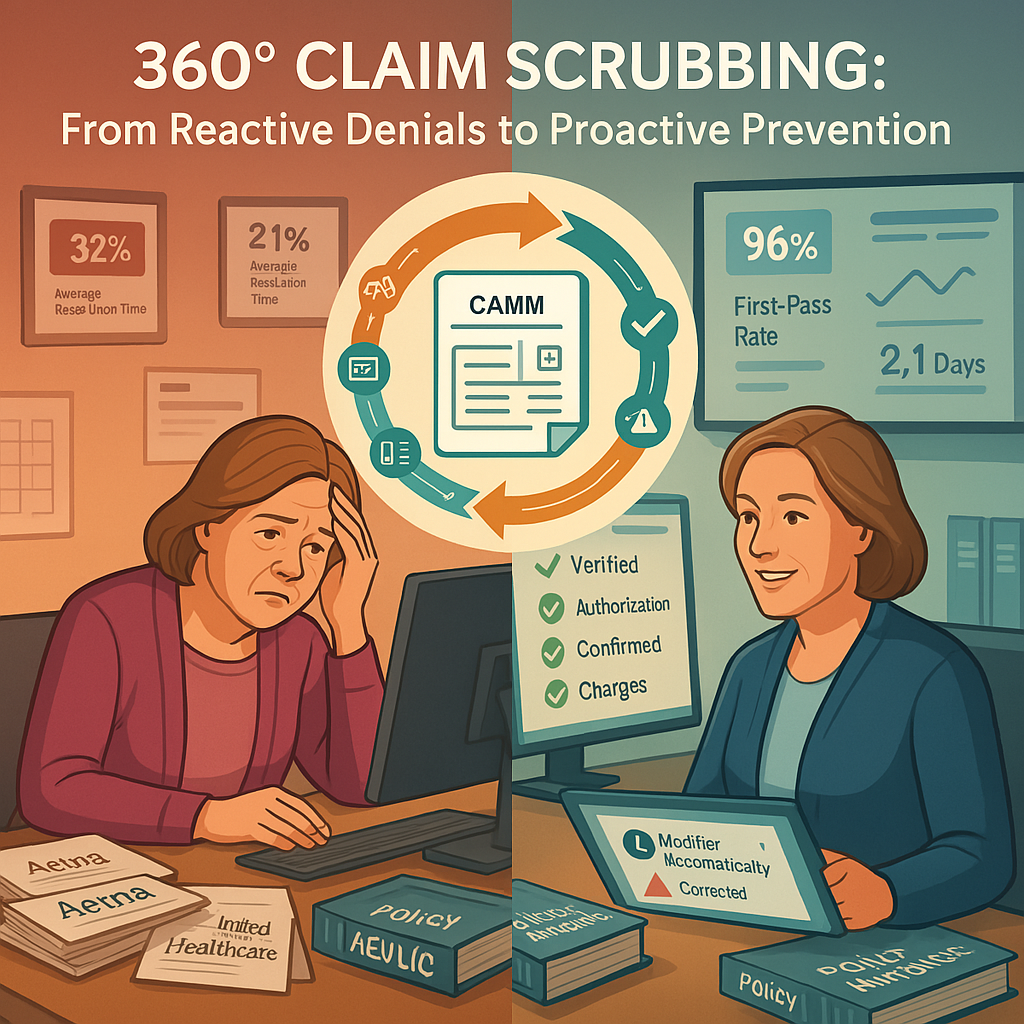
Denial management involves a systematic approach to identifying why claims are denied, correcting the issues, and resubmitting the claims for reimbursement. Common reasons for claim denials include coding errors, missing information, incorrect patient data, and issues related to insurance coverage. Effective denial management not only recovers lost revenue but also helps in identifying patterns and root causes of denials, thereby preventing future occurrences.
Proactive Denial Management
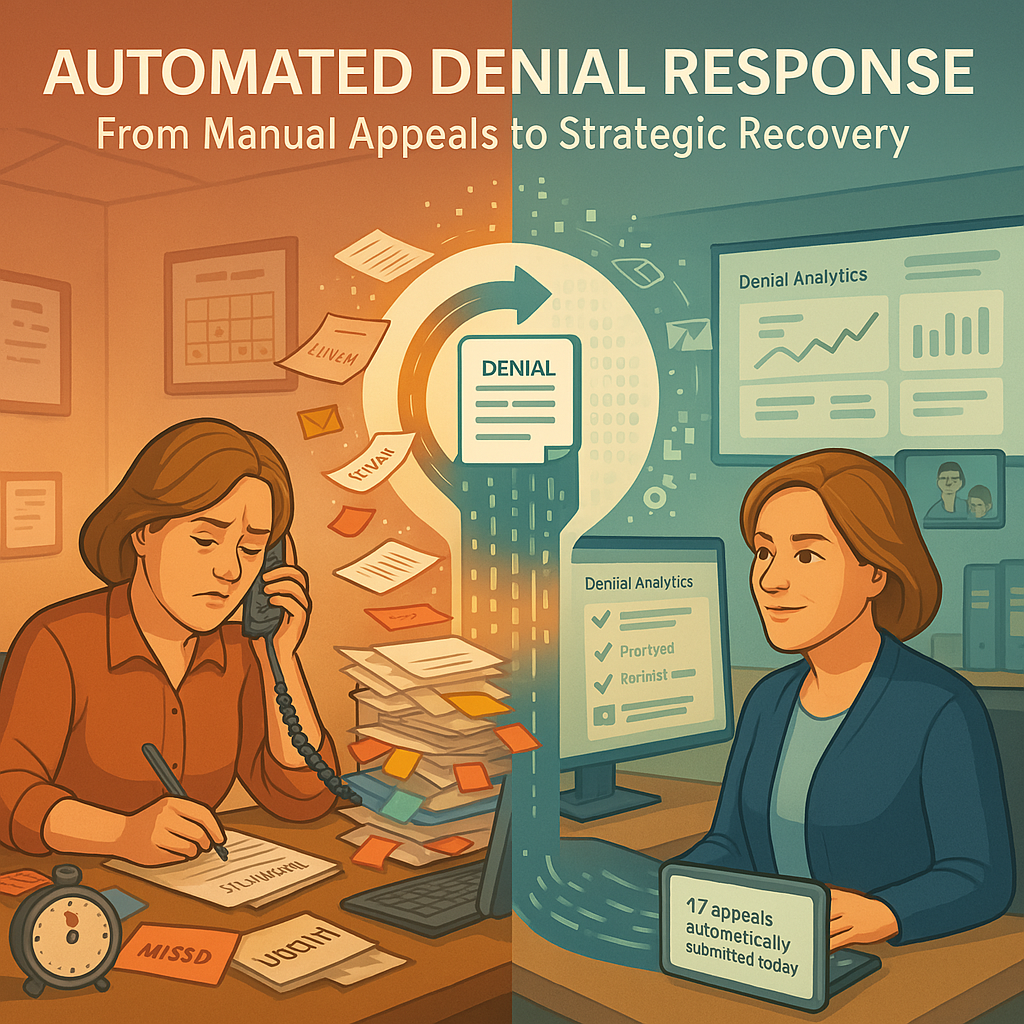
Managing denials effectively is crucial for efficient RCM. Revenue cycle directors need to dissect each denial individually to understand underlying issues. This proactive approach helps identify and address repetitive errors, improving overall efficiency.
- Detailed Denial Management Reviews: Analyzing each denial categorically can reveal common issues leading to denials, such as procedural discrepancies or staff misunderstandings about insurer requirements. Creating checklists based on these insights can prevent future errors.
- Targeted Staff Training: Providing training sessions tailored to specific denial issues empowers staff to handle future cases better. Emphasizing the impact of their roles on financial outcomes through data-driven insights is key.
Precision Tactics for Denial Resolution
- Data-Driven Analysis: Utilizing advanced data analytics to identify trends and patterns in denials can significantly enhance the precision of denial management. By analyzing historical data, healthcare organizations can predict the likelihood of certain types of denials and proactively address potential issues.
- Customized Workflows: Developing customized workflows for different types of denials can streamline the resolution process. For instance, claims denied due to coding errors can follow a different workflow than those denied for eligibility issues. Tailoring workflows ensures that the right resources are allocated to resolve each denial efficiently.
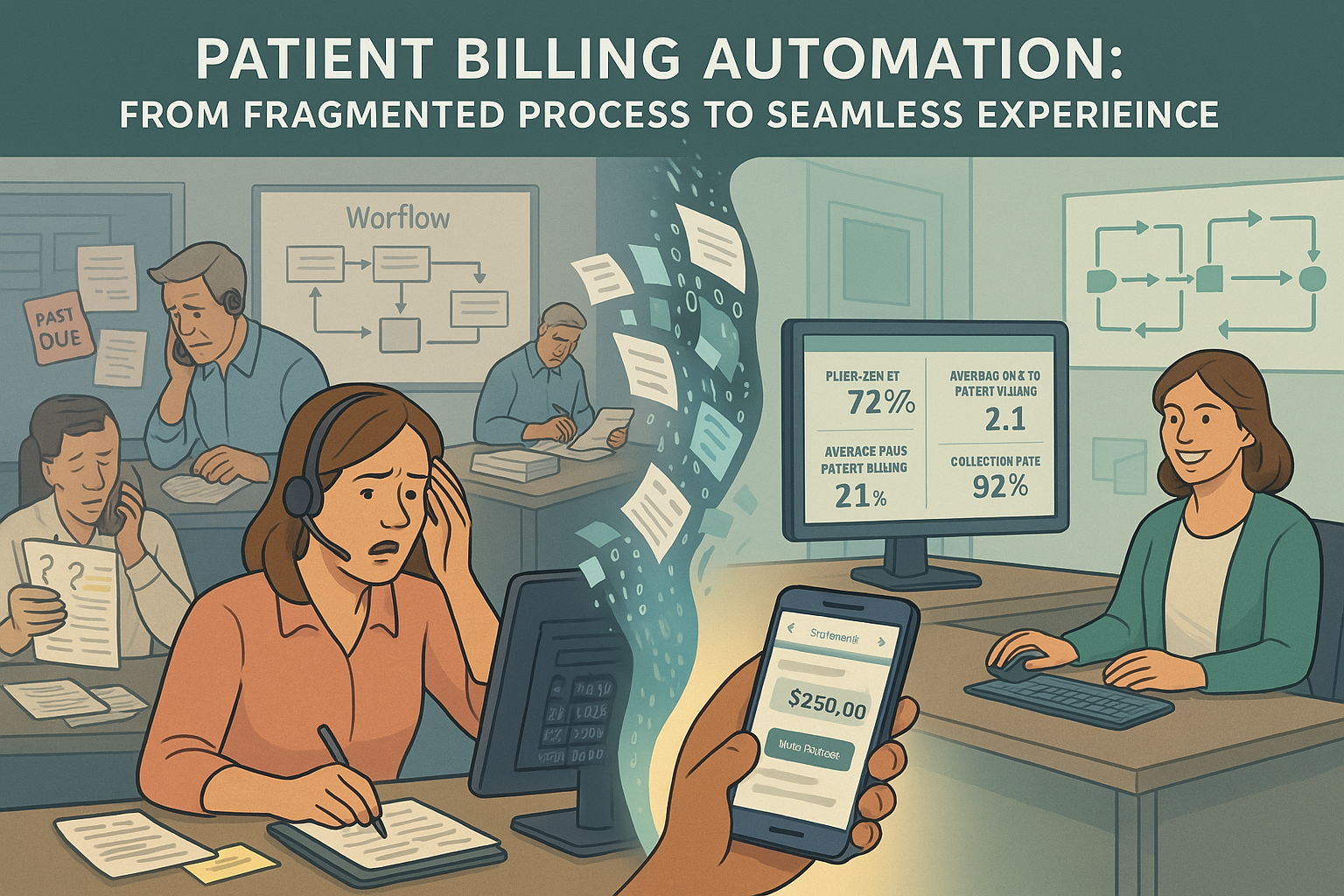
- Advanced Automation: Implementing automation tools, such as artificial intelligence (AI) and machine learning (ML), can expedite the denial management process. These technologies can automatically flag potential denials, suggest corrective actions, and even resubmit claims with minimal human intervention. Automation not only speeds up the process but also reduces human error.
- Education and Training for Denial Management: Regular training for billing and coding staff on the latest payer requirements and coding standards is crucial. Personalized training programs that address common errors and specific challenges faced by the staff can significantly reduce the rate of denials.
- Patient-Centric Approaches: Involving patients in the denial resolution process can also be beneficial. Educating patients about their insurance coverage and the necessary documentation can prevent denials related to incomplete or incorrect information. Personalized patient communication strategies, such as tailored reminders and follow-ups, can improve the accuracy of the information provided.
Team Communication in Denial Management
Effective communication is crucial, especially between different segments of the RCM process. Ensuring clear and continuous communication helps in bridging gaps.
- Regular Meetings: Conducting regular meetings, including daily stand-ups for immediate concerns and weekly strategic sessions, ensures all team members are aligned and informed about their roles in addressing challenges.
- Modern Communication Tools: Utilizing modern communication tools like real-time messaging apps or collaborative platforms can replace outdated methods like emails. These tools are essential for enhancing interactions, especially with remote or offshore teams.
Strategic Conversations Without Blame
Handling discussions about errors or inefficiencies in RCM processes requires tact and a focus on constructive improvement rather than blame.
- Collaborative Problem Solving: Encouraging team members to contribute solutions to operational challenges fosters a sense of ownership and can lead to innovative improvements directly from those handling the tasks.
- Empathetic Feedback: Providing feedback in a supportive manner, focusing on systems and processes rather than individuals, helps maintain team morale and promotes a culture of continuous improvement.
Conclusion
Refining RCM efficiency involves more than just technological upgrades or outsourcing. It requires a strategic focus on managing denials and improving team communication. By focusing on these areas, RCM leaders can enhance operations, improve staff engagement, and achieve better financial outcomes. By leveraging data-driven analysis, customized workflows, advanced automation, and enhanced communication, healthcare organizations can address the root causes of denials more effectively. The shift towards precision tactics not only boosts revenue recovery but also enhances operational efficiency and patient satisfaction. As healthcare continues to evolve, adopting personalized denial management strategies will be essential for financial sustainability and delivering high-quality patient care.