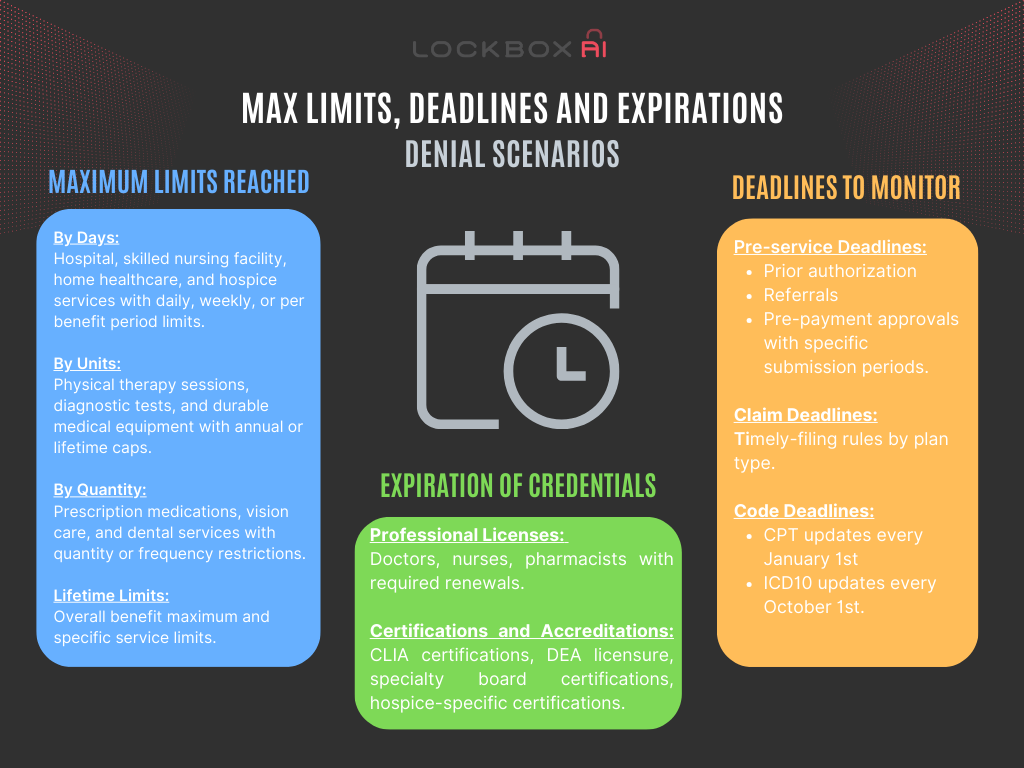
Effective denial management in RCM is crucial for ensuring the financial health of healthcare organizations. Denials, whether from payers or patients, can significantly impact revenue streams and operational efficiency. Understanding the key limits, deadlines, and expirations associated with denial management is essential for healthcare providers to optimize revenue capture and minimize revenue loss. A crucial part of RCM is denial management, which involves identifying, managing, and preventing claims denials to ensure the financial health of a healthcare provider. Effective denial management requires a deep understanding of key limits, deadlines, and expirations. This article explores these elements in detail, highlighting the importance of Denial Management in RCM. Maximum Benefits Limits are often reached unknowingly until that claim denial comes in. There are various deadlines to be aware of throughout the life of a claim or care of a patient.
Understanding Denials in RCM
Denials occur when an insurance company refuses to honor a request to pay for healthcare services. They can be due to various reasons, including incomplete or inaccurate information, coding errors, lack of medical necessity, or issues related to coverage. Effective denial management in RCM involves addressing these issues promptly to minimize revenue loss.
Here’s a breakdown of the most common limits, deadline and expirations that trigger denials:
Maximum Limits Reached in Denial Management in RCM
By Days:
- Hospital stays: Many plans have limits on the number of days covered for inpatient stays, with possible extensions for medically necessary reasons. Some plans may allow for annual or lifetime limits on hospital days. (Renewable in some cases with medical justification)
- Skilled nursing facility stays: Similar to hospital stays, some plans have limits on covered days in skilled nursing facilities, with potential extensions for medically necessary reasons. Annual or lifetime limits might also apply. (Renewable in some cases with medical justification)
- Home healthcare services: Some plans have daily or weekly limits on home healthcare services, like physical therapy or home nursing visits. These limits might be renewable depending on the plan and medical needs.
- Hospice Services: For patient eligibility in Medicare-covered hospice care, a physician needs to certify the patient’s terminal illness, with recertification required for each benefit period (usually 60 days).
By Units:
- Physical therapy sessions: Plans may have limits on the number of covered physical therapy sessions per year or treatment plan. Renewals might be possible with medical justification.
- Diagnostic tests in denial management in RCM: Some plans have limits on the number of covered diagnostic tests, like MRIs or CT scans, per year. Renewals may be allowed depending on the plan and medical needs.
- Durable medical equipment (DME): Some plans have limits on the number of DME items covered, like wheelchairs or nebulizers, per year or lifetime. Renewals may be possible based on equipment wear and tear or changes in medical needs.
By Quantity:
- Prescription medications: Some plans have limits on the quantity of certain medications covered per prescription or per year. Renewals may be allowed depending on the medication and medical needs.
- Vision care: Plans may have limits on the frequency of covered eye exams or the amount covered for glasses or contacts per year. Renewals might be possible depending on the plan and changes in vision.
- Dental services: Some plans have limits on the number of covered dental procedures per year or lifetime. Renewals may be possible depending on the plan and dental needs.
Lifetime Limits:
- Overall benefit maximum: Some plans have a lifetime maximum benefit amount for all covered services, after which no further coverage is provided. This is usually a very high limit. (Not renewable)
- Specific service limits: Some plans have lifetime limits for specific services, like organ transplants or certain surgeries. These limits are often non-renewable.
- Limit Renewal Possibilities: Generally, limits associated with medical necessity (hospital stays, skilled nursing facility stays, home healthcare) have higher chances of renewal with proper documentation
Deadlines to Monitor in Denial Management in RCM
Pre-service Deadlines:
- Prior Authorization: Timeframes for submitting and receiving prior authorization for specific procedures or medications. Missing deadlines can result in denied claims or delayed payment.
- Referrals: Validity periods for referrals from primary care physicians to specialists. Expired referrals might lead to denied claims for subsequent services.
- Pre-payment approvals: Some plans require pre-payment approval for certain services, with specific deadlines for submission. Missing deadlines could delay payment or deny the claim.
Codes and Claims Deadlines:
- Claim submission deadlines: Most insurers allow 12 months from the date of service for claim submission. Submitting within 90 days is recommended for faster processing and minimizing denial risks.
- Appeals deadlines: Typically 60-90 days after receiving a denial notification. Act promptly to avoid missing the deadline and losing your appeal right.
Expiration of Credentials
- Professional licenses: Medical professionals like doctors, nurses, and pharmacists must maintain their licenses through continuing education and renewal fees. Claims for services provided by unlicensed or unrenewed professionals could be denied.
- CLIA certification: As you mentioned, Clinical Laboratory Improvement Amendments (CLIA) certification for labs expires every two years. Claims from non-certified labs are likely denied.
- DEA licensure: Drug Enforcement Administration (DEA) licenses for controlled substances expire every three years. Claims submitted by physicians without valid licenses could be denied.
- Specialty board certifications: Many medical specialties have board certifications that expire and require recertification periodically, often every 10-15 years, with continuing education and re-examination.
Hospice-Specific Providers:
- Individual Certifications: Many hospice staff members, like nurses and social workers, need certifications specific to hospice and palliative care. These are offered by organizations like the Hospice and Palliative Credentialing Center (HPCC). Recertification is required to maintain these credentials, typically every few years.
- Physician Certification: Physicians working in hospice might have certification from the American Academy of Hospice and Palliative Medicine. Specific requirements vary.
- Hospice Accreditation: The hospice organization itself undergoes accreditation by agencies like The Joint Commission. Accreditation ensures the hospice meets quality standards and is renewed periodically.
Between internal deadlines, external compliance requirements, and expirations for various authorizations and insurances, it’s easy to miss something. By using every tool at your disposal, you can set up automated flags and reminders to ensure you never miss these denial triggers.
Conclusion
Denial management is a vital part of Revenue Cycle Management, requiring careful attention to key limits, deadlines, and expirations. By understanding and effectively managing these elements, healthcare providers can minimize revenue loss, ensure timely reimbursement, and improve overall financial performance. Implementing proactive strategies, regular training, and leveraging technology are essential steps in optimizing denial management processes. Effective Denial Management in RCM is not just about responding to denials but preventing them, ensuring the financial health and operational efficiency of healthcare providers.