Patient Referral : Challenges for PCPs and Specialists
As a claims denial manager, there’s nothing quite like a perfectly coded claim getting tossed aside because of a missing patient referral. Let’s break down the denial causes that start with the referring providers and extend to the specialists.
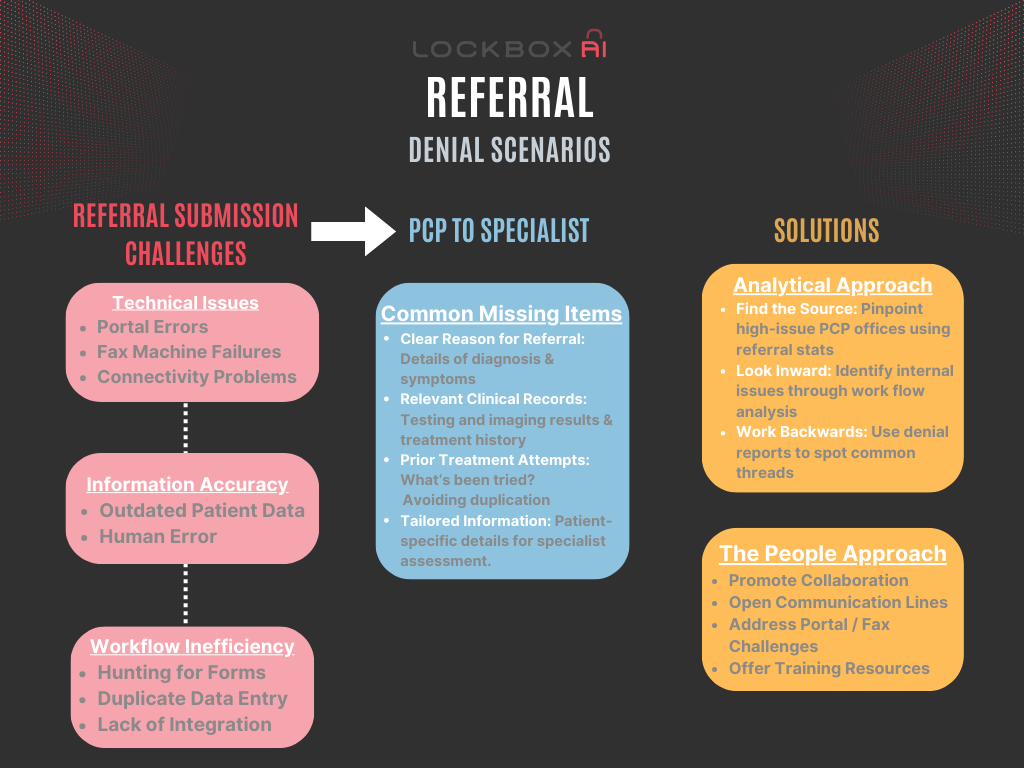
Patient Referral Submission: Roadblocks to the Process
- Technical Issues:
-
-
- Portal Errors: Insurance portals can have glitches, bugs, or compatibility issues that crash mid-submission or corrupt data, forcing the PCP to start over.
- Fax Machine Failures: If relying on fax, malfunctions or busy signals interrupt transmission making it hard to confirm a referral was received.
- Connectivity Problems: Poor internet connection can disrupt online form submissions, leading to timeout errors and data loss.
-
- Information Accuracy:
-
-
- Outdated Patient Data: Incorrect insurance information, policy numbers, or addresses cause immediate rejections, requiring the PCP to locate the correct details.
- Human Error: Simple typos in names, dates, or medical codes can lead to submission failures or mismatches, demanding careful review before hitting “submit.”
-
- Workflow Inefficiency:
-
- Hunting for Forms: Locating the correct, up-to-date form for a specific insurance company can be a hunt through websites or disorganized files.
- Duplicate Data Entry: PCPs may need to re-enter the same patient information across multiple systems for different referrals or follow-up communications.
- Lack of Integration: Switching between their practice’s electronic health records (EHR) system and disparate insurance portals disrupts smooth workflow.
PCP to Specialist: Common Missing Items
- Clear clinical reason for patient referral: The specialist might need a more detailed explanation of the patient’s diagnosis, symptoms, and why the referral is necessary.
- Relevant medical records: Test results, imaging studies, and past treatment history from the referring provider can aid the specialist in evaluating the patient.
- Prior treatment attempts: The specialist may want to know what medications or therapies the patient has already tried, to avoid duplication and understand the case better.
- Specific questions: Sometimes the specialist might have particular information they need to properly assess the patient’s needs or determine appropriate next steps.
Administrative Hurdles
Navigating the administrative maze of patient referrals can be a daunting task for healthcare providers. From obtaining prior authorizations to coordinating appointments, the administrative burden associated with referrals can consume valuable time and resources. Streamlining administrative processes and leveraging technology solutions can help alleviate this burden and improve the efficiency of the referral process.
Access Barriers
Limited access to specialty care services presents a major barrier to patient referrals. Long wait times, geographic disparities, and insurance constraints can hinder patients’ ability to receive timely and appropriate care from specialists. Addressing these access barriers requires innovative solutions, such as telehealth services, community-based care models, and increased investment in underserved areas.
Quality Assurance
Ensuring the quality and appropriateness of patient referrals is paramount to delivering high-quality healthcare. PCPs must possess the necessary knowledge and expertise to make informed referral decisions, while specialists must uphold rigorous standards of care in their evaluation and treatment of referred patients. Continuous education, clinical guidelines, and peer review mechanisms can help uphold quality standards throughout the referral process.
Patient Empowerment
Empowering patients to actively participate in the referral process is key to improving outcomes and enhancing patient satisfaction. Educating patients about their healthcare options, involving them in decision-making, and providing access to resources and support can help empower individuals to navigate the complex landscape of referrals with confidence and autonomy.
Other Ways Patient Referral Get Complicated
Even when everything seems to go smoothly, there are hidden roadblocks:
- The Time Crunch: Sometimes, a patient needs a specialist urgently. The referral process, however, can take days or even weeks, leaving the patient in limbo and potentially delaying critical care. There’s simply no time for a slow and bureaucratic dance.
- Communication Breakdowns in Patient Referral: Miscommunication between the PCP’s office, patient, and insurance company is a recipe for disaster. A dropped referral, a missed follow-up call, or a simple misunderstanding about what information is needed can derail the entire process.
- The Payor Variety: Here’s where things get interesting. Insurance plans have different rules for referrals. Medicare and Medicaid generally don’t require them, but let’s look at some popular private plans:
- HMOs (Health Maintenance Organizations) typically require referrals for almost everything except seeing your PCP.
- PPOs (Preferred Provider Organizations) usually offer more flexibility, but referrals might still be needed for certain specialists or services.
- POS (Point-of-Service) plans can be a mix of HMO and PPO features, so referral requirements can vary depending on the specific plan design.
- EPOs (Exclusive Provider Organizations) require referrals to see any in-network provider, similar to HMOs.
There’s also the added complexity of referral requirements:
- The Expiration Rules: As if all that wasn’t enough, most referrals have expiration dates. If the patient doesn’t schedule the appointment within that time frame or switches insurance plans mid-care, the whole process has to start over again.
- Doubtful Backdating: Forget about convincing the insurance company to backdate an authorization. Their answer is very often a “no,” leaving either the patient or the specialist to take the hit.
Reducing Patient Referral Denials: Can Anything Be Done?
So, what can we do to stop the madness? Here are some actionable steps:
- Finding the Source: Analyze denial reports to pinpoint PCP offices with frequent referral-related denials. This isn’t about pointing fingers – it’s about identifying trends.
- Collaboration, Not Confrontation: Open communication is key. Discuss challenges PCP referral coordinators face with your online portal or fax system. Are there any additional resources or training materials we could provide to ensure referrals are processed smoothly?
- Looking Inward: Are faxes managed efficiently? Are referral numbers entered correctly on claims? Analyze denials to see if the issue might lie within your organization.
- Working Backwards: Use analytics to identify the line of service most denied due to missing referrals. Then, work backwards to see if there are any common threads among these denials. For example, are they all referrals for a specific type of specialist or service?
Your denial reports hold the key. Unlock their insights together. Clear communication across internal teams as well as with referral sources is crucial to reduce denials and ensure patients get the care they deserve.
Conclusion
Patient referrals serve as vital conduits for delivering specialized care and optimizing patient outcomes. However, numerous challenges stand in the way of seamless referral processes, ranging from communication barriers and administrative complexities to access limitations and quality assurance concerns. Addressing these challenges requires a concerted effort from healthcare stakeholders to streamline processes, enhance communication, and prioritize patient-centered care. By working together to overcome these obstacles, PCPs and specialists can ensure that patients receive the timely, appropriate, and high-quality care they deserve.