Taking Control of Duplicate Claim Denials
Duplicate claim denials are a persistent headache for healthcare Revenue Cycle Management (RCM) teams. These denials can be frustrating because sometimes they reflect true duplication in submission for unfortunate reasons, while other times, the payer has never adjudicated the initial claim. Let’s look at reasons why claims get flagged as duplicates.
Understanding Duplicate Claim Denials
Duplicate claim denials occur when a healthcare provider submits multiple claims for the same service or procedure for the same patient within a specific timeframe. These duplicate submissions can result from various factors, including system errors, billing software glitches, or human error. While some duplicate claims may be unintentional, others can be the result of fraudulent activities aimed at maximizing reimbursement.
Healthcare payers, including insurance companies and government programs such as Medicare and Medicaid, have stringent guidelines and protocols in place to prevent duplicate payments for the same services. When duplicate claims are detected, payers typically deny the subsequent claims and request additional documentation or justification for the billing discrepancies. This can lead to delays in payment processing and create administrative burdens for healthcare providers.
Challenges Faced by Healthcare Providers
Duplicate claim denials pose several challenges for healthcare providers, including:
- Revenue Loss: Denied claims result in delayed or reduced reimbursement, leading to financial losses for healthcare organizations. The time and resources spent on reprocessing denied claims further exacerbate the financial impact.
- Administrative Burden: Dealing with duplicate claim denials requires significant administrative effort, including identifying the root causes of the duplicates, resubmitting claims, and communicating with payers to resolve the issues. This diverts resources away from patient care and other critical tasks.
- Compliance Risks: Persistent duplicate claim denials can raise red flags for payers and regulatory agencies, potentially triggering audits and investigations into the provider’s billing practices. Non-compliance with billing regulations can result in fines, penalties, and damage to the provider’s reputation.
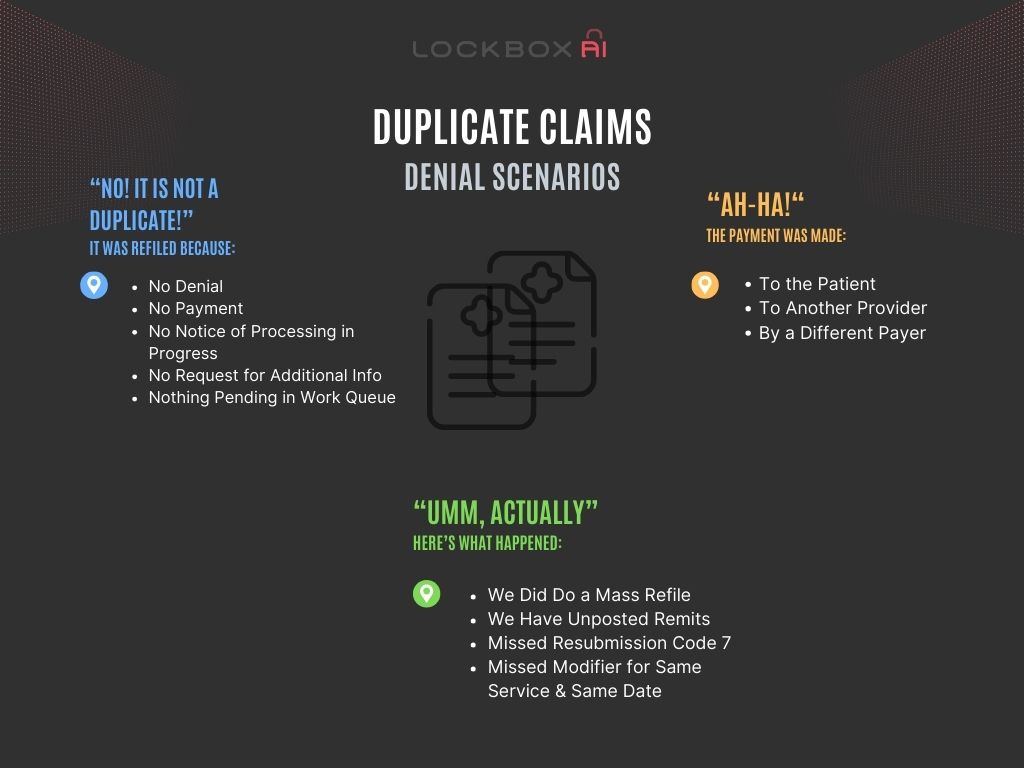
True Duplicates: When Two Claims Are One Too Many
- Mass Refiling: Sometimes, busy RCM teams might resubmit a bunch of claims all at once without carefully checking each one first. This “shotgun approach” can lead to a lot of true duplicate submissions.
- Posting Delays: Delays in getting denials or payments recorded in the system can cause problems. A claim might appear unprocessed for days, leading someone to resubmit it, only to find it was already denied or paid (but yet reflected in the system).
- Lost Remittances: Remittance Advices (like Explanation of Benefits forms) explain how a payer processed a claim. If one of these goes missing, the provider might not know a claim was already processed and could resubmit it as a duplicate.
- Queue Backlog in Duplicate Claim Denials: If the RCM team is overloaded with claims, it can be hard to keep track of everything. A claim waiting to be reviewed might be accidentally resubmitted, resulting in a duplicate.
- Payment In Process: Even when a claim is processed, it can take some time for the payment to reach the provider. A claim resubmitted during this waiting period might be flagged as a duplicate.
False Duplicates: When It’s Not Really a Duplicate But…
Reasons claims are not a duplicate but get identified as such can often be prevented. A couple of examples are:
- Missing Modifiers: Modifiers used to explain why the same service was provided by the same provider on the same day may have been missed. Failing to attach these modifiers to the proper service will cause it to be denied as a duplicate service.
- Corrected Claim Identifier: During corrected claim submissions, forgetting to use Code 7 identifier will cause the payer to classify it as the same claim sent again. This code tells the payer the claim is a correction; leaving it out is a common reason for duplicate denial.
Missing Remit Notices Fuels Duplicate Claim Submissions
- Missing Denial Notices: Delays or a complete lack of communication from payers regarding claim status can leave providers in the dark. Without proper notice, the RCM team will default to resubmitting the claim if a status check is not the first course of action of a company’s RCM policy and protocols.
Avoiding Double Work: Strategies for Smoother Workflows
These tangled workflows and failed communication can create a lot of extra work for RCM teams. Here are some tips to minimize the volume of duplicate denials:
- Accurate Coding: Make sure the team is using the right codes and modifiers on all claims.
- Organized Queues: Use a system where claims statuses are worked in the order that coincides with other departments.
- Investigate Duplicate Claim Denials: Perform claim status checks on all unadjudicated claims and save the automatic refiling protocol to clusters of claims that have fallen through the cracks.
- Detailed Electronic Notes: Make detailed notes on all touched claims, a mandatory rule. Encourage clear communication of claims status to the rest of the team at all times.
No one has the time to touch the same claim more than once needlessly. By implementing these strategies, RCM teams can minimize self-inflicted duplicate denials and focus their energy on those beyond their own control.
Conclusion
Duplicate claim denials present significant challenges for healthcare providers, impacting revenue, increasing administrative burdens, and exposing organizations to compliance risks. By implementing proactive strategies such as enhancing billing systems, implementing clear policies and procedures, conducting regular audits, and utilizing electronic health records, providers can take control of duplicate claim denials and optimize their revenue cycle management processes. By prioritizing accuracy, compliance, and efficiency in billing practices, healthcare organizations can minimize financial losses, improve operational efficiency, and enhance the overall quality of patient care.