The Credentialing Process: A Team Effort to See Patients Faster
Introduction
The credentialing process is a critical component of healthcare that ensures providers are qualified to deliver safe and effective care. However, this process can often be time-consuming and complex, leading to delays in patient access to necessary services. To address these challenges, healthcare organizations are increasingly recognizing that credentialing is a team effort. By fostering collaboration among various stakeholders, organizations can streamline the credentialing process, ultimately enabling patients to receive care more quickly.
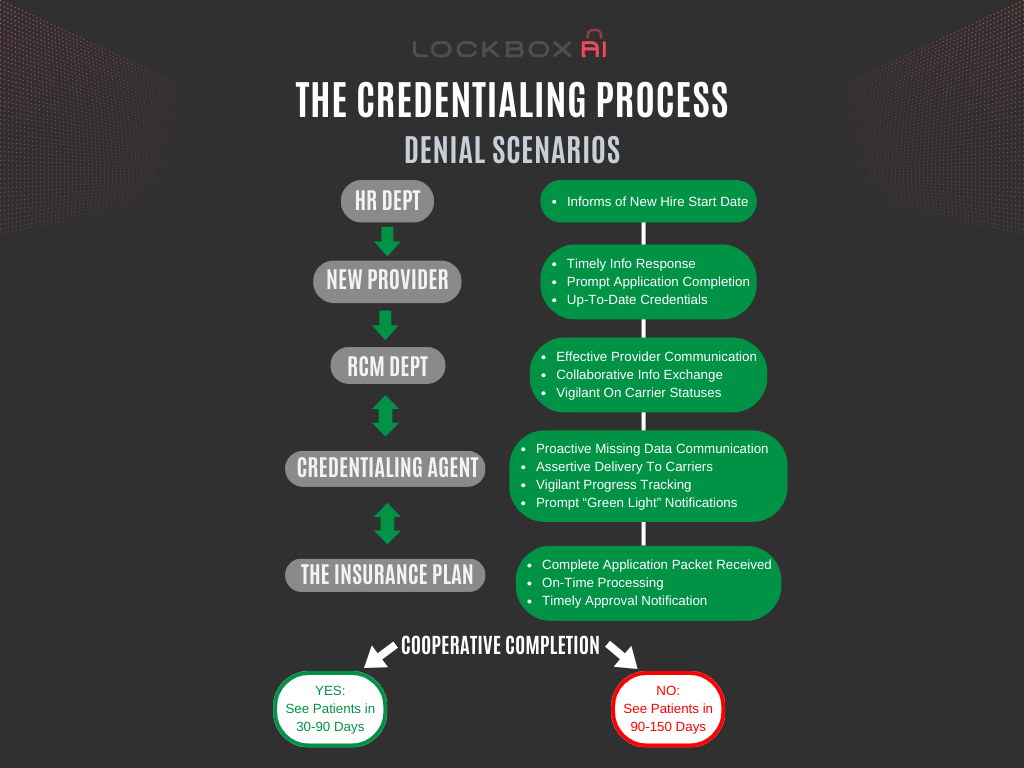
A new healthcare provider joins your team – great news! But before they can welcome patients, they need to complete credentialing, a vital process that verifies their qualifications for insurance participation. Here’s a breakdown of how different departments (or combined departments) can work together to ensure a smooth and efficient credentialing process, getting providers seeing patients sooner.
Onboarding – Setting Clear Expectations
The journey starts with a well-informed HR department:
- Introduction to Credentialing: Upon hiring, HR explains the credentialing process to the new provider, emphasizing its importance for the start of patient care.
- The Credentialing Contact: HR introduces the provider to their primary contact – either the dedicated Credentialing department or the RCM (Revenue Cycle Management) department, which may handle credentialing in some organizations.
The RCM Department – Gathering Credentials in Healthcare Organizations
The RCM department, whether handling credentialing or not, plays a crucial role:
- Initial Contact: They promptly reach out to the provider to collect a signed enrollment application and essential credentials like CVs, licenses, and DEA certificates.
- Clear Communication: The RCM team maintains open communication with the provider, keeping them updated on progress and any outstanding information needed.
- Handoff to Credentialing (if separate): Once they have a complete application package, the RCM department seamlessly transitions it to the credentialing team (if credentialing is a separate department).
- Setting Realistic Timelines: The provider is given a realistic timeline (45-90 days) while acknowledging potential delays due to insurance turnaround times.
The Credentialing Department – Navigating Payer Requirements in Healthcare Organizations
The credentialing team takes the application and tackles the legwork with insurance companies:
- Application Preparation and Submission: They meticulously prepare and submit applications to each relevant health plan the provider wishes to participate in.
- Tracking Applications in Healthcare Organizations: The team utilizes a robust tracking system to monitor the status of each application with every payer.
- Proactive Communication in Healthcare Organizations: They identify and address any missing information requests or delays from insurance companies to prevent application holdups.
The Insurance Plans – Rule The Day:
- Timely Response: Insurance plans grant final approval. Prompt responses to inquiries and clear communication regarding missing information or additional requirements are a must. Turnaround times that prevent the provider from hitting the intended start date result in lost revenue and delays to patient care.
- Standardized Processes in Healthcare Organizations : Consistent and transparent credentialing procedures across different plans would greatly simplify the process for everyone.
Waving the Green Flag – Tell One, Tell All
After weeks of diligent work, approvals start rolling in from each payer, the credentialing team must promptly inform the RCM department and the appointment schedulers of each approval, confirming in-network status with specific health plans.
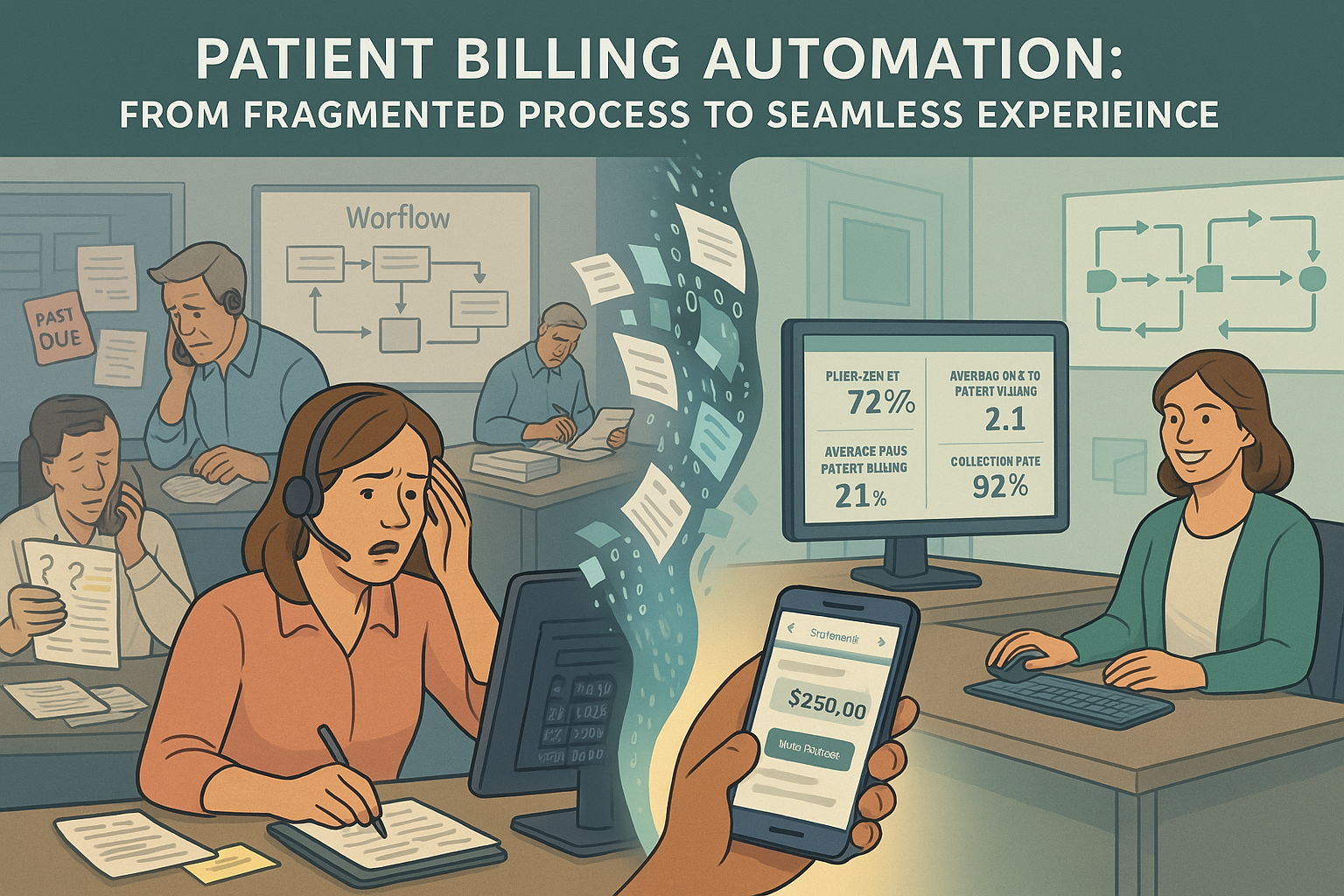
Credentialing Denials – The Financial Impact: Without proper credentialing, submitted claims will be denied by insurance companies. Here are a few common reasons:
- Provider Out-of-Network (Choice): The healthcare organizations may choose not to participate with a specific health plan, rendering the provider out-of-network for those patients.
- Provider Out-of-Network (Timing): Claims are submitted before the credentialing application is completed and approved, resulting in an out-of-network status at the time of service.
- Missing or Expired Credentials: Required licenses or certifications were either not submitted or expired during the application process.
Working Together Towards a Seamless Process in Healthcare Organizations
By collaborating effectively, different departments can significantly improve the credentialing process:
- Technology as a Partner: Investing in credentialing management software can streamline application assembly, track progress with each payer, and automate tasks.
- Open Communication Channels in Healthcare Organizations: Regular communication between HR, RCM, credentialing (if separate), and the provider ensures everyone is on the same page and aware of any roadblocks.
- Standardized Applications: Advocating for standardized credentialing requirements across health plans can ease the burden on providers, reducing the likelihood of missing information.
A well-coordinated credentialing journey isn’t just about paperwork; it’s about ensuring timely access to qualified healthcare providers. By fostering collaboration, clear communication, and utilizing technology, healthcare organizations can get providers seeing patients efficiently, ultimately delivering uninterrupted care to their patients.
Conclusion
The credentialing process is essential for ensuring the safety and quality of patient care. By embracing a team-oriented approach, healthcare organizations can streamline this process, reducing delays and improving patient access to care. Collaboration among credentialing specialists, medical staff leaders, HR, IT, and legal teams not only enhances efficiency and accuracy but also fosters a culture of communication and support. As technology continues to evolve, integrating digital solutions into the credentialing process will further empower teams to meet the growing demands of healthcare delivery, ultimately benefiting both providers and patients alike.