In today’s rapidly evolving healthcare landscape, the Revenue Cycle EHR Crisis looms large, posing significant challenges to the industry. It’s imperative for healthcare providers to adapt and embrace technological change to navigate through this crisis effectively.
Understanding the EHR Crisis
The EHR crisis refers to the challenges and shortcomings associated with the adoption and utilization of electronic health records in healthcare settings. While EHR systems offer numerous benefits, including improved efficiency and accessibility of patient information, they also present significant hurdles such as interoperability issues, usability concerns, and data security risks.
Key Components of the EHR Crisis
- Interoperability Challenges: Incompatibility between different EHR systems impedes the seamless exchange of patient data among healthcare providers.
- Usability Issues: Complex interfaces and cumbersome workflows hinder user adoption and efficiency, leading to dissatisfaction among healthcare professionals.
- Data Security Risks: The digitization of health records introduces vulnerabilities to cyber threats and unauthorized access, raising concerns about patient privacy and confidentiality.
Impact of the Revenue Cycle EHR Crisis
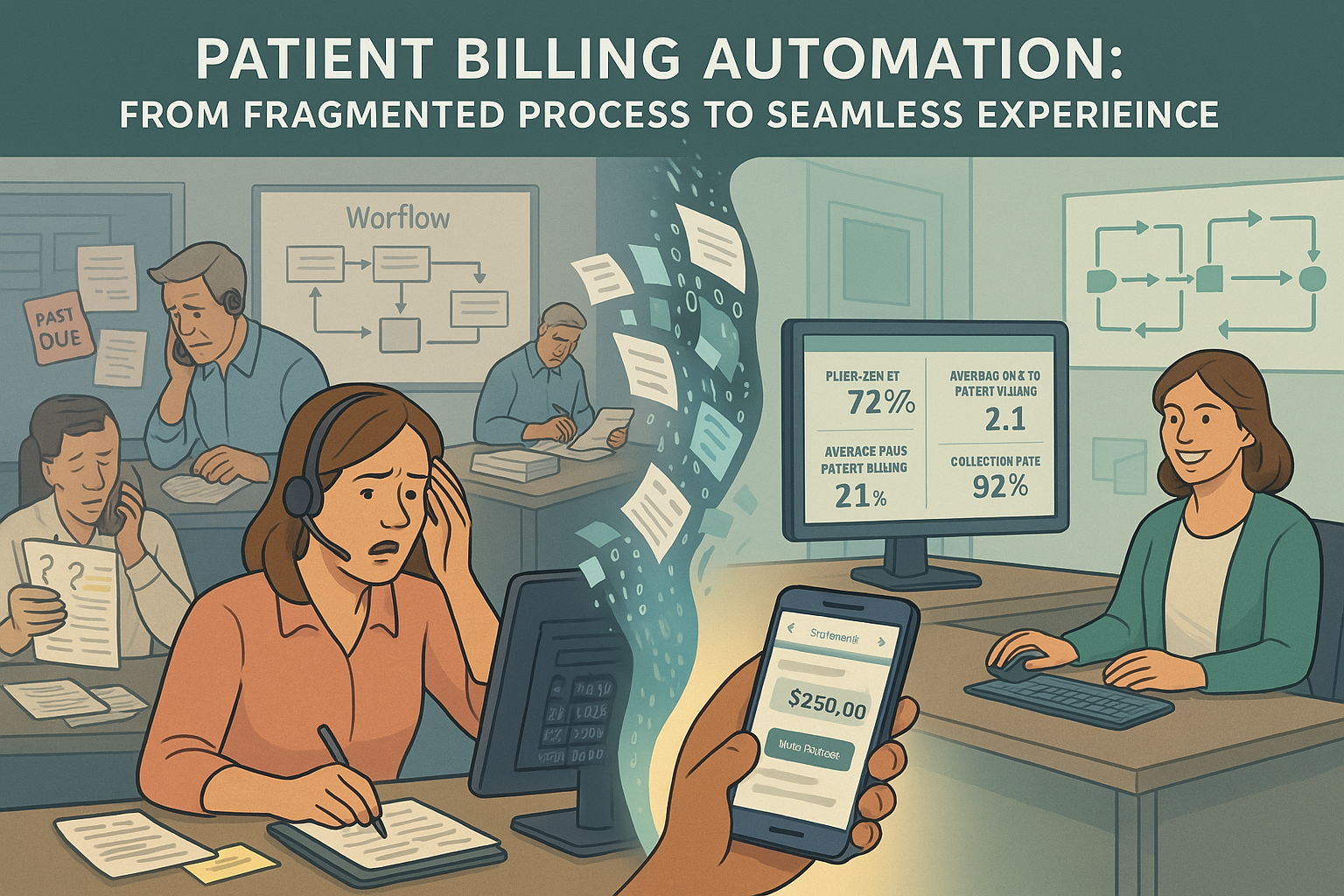
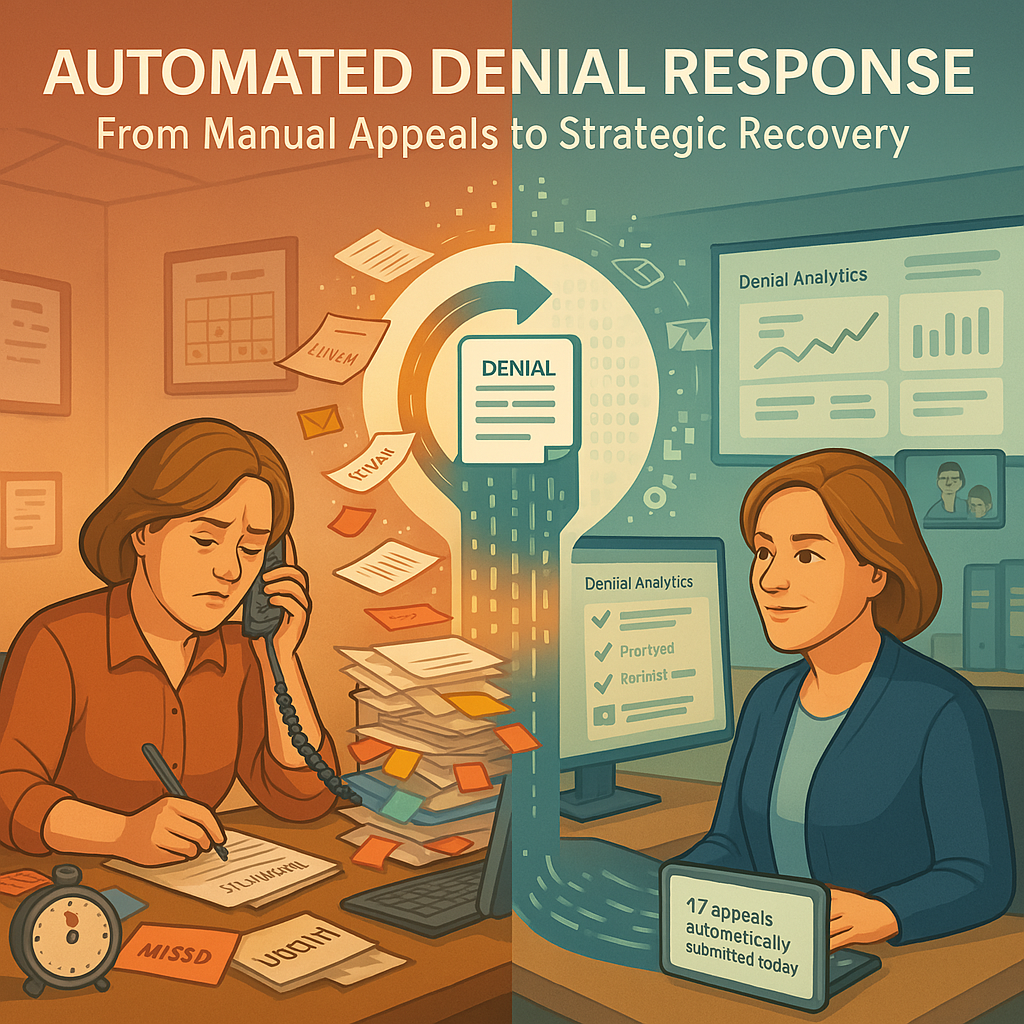
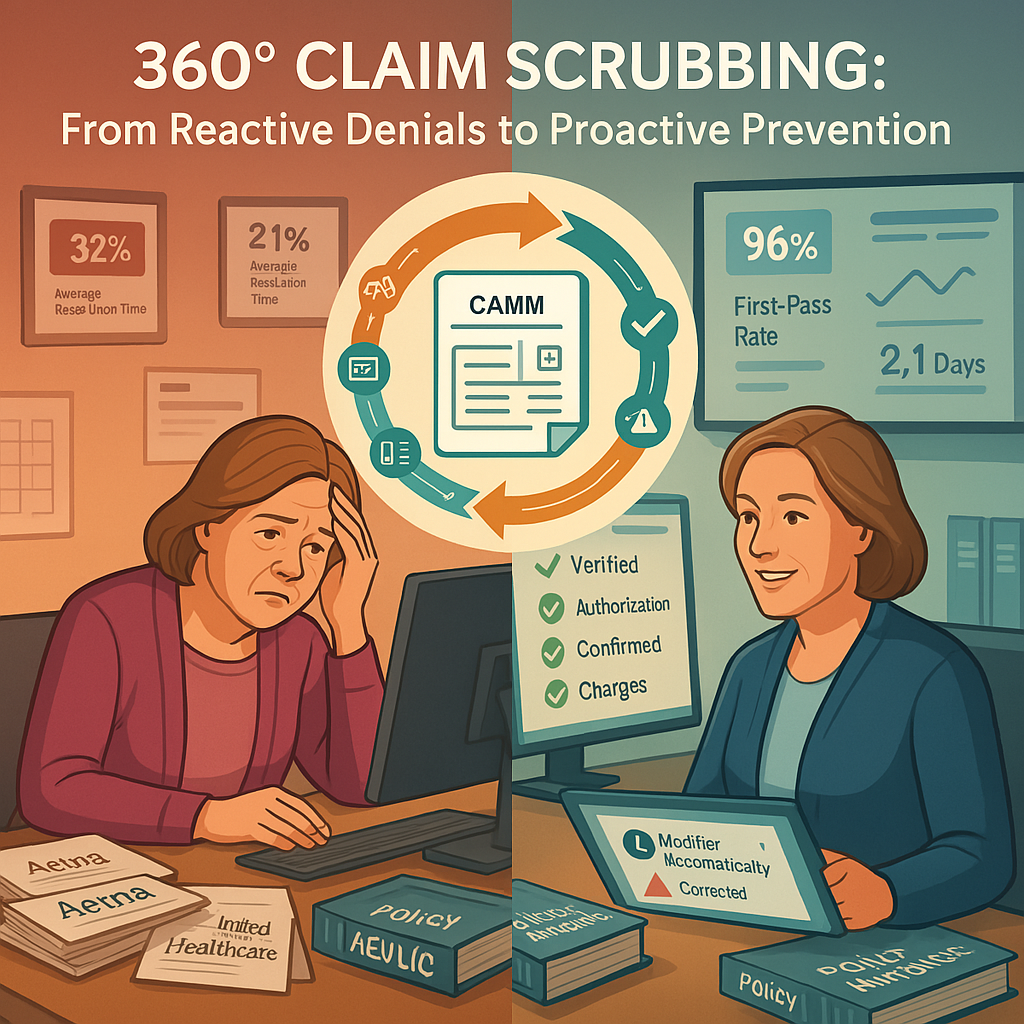
The revenue cycle EHR crisis exacerbates financial challenges for healthcare organizations, affecting their bottom line and ability to provide quality care. Inefficient revenue cycle management processes, coupled with the shortcomings of EHR systems, contribute to billing errors, claim denials, and revenue leakage.
Consequences of the Revenue Cycle EHR Crisis
- Financial Strain: Revenue cycle inefficiencies lead to delayed payments, increased administrative costs, and decreased profitability for healthcare providers.
- Patient Dissatisfaction: Billing errors and insurance claim denials frustrate patients, eroding trust and satisfaction with healthcare services.
- Operational Burdens: Manual billing processes and data entry tasks divert valuable resources and manpower away from patient care activities.
The Need for Technological Change
To address the EHR crisis and improve the efficiency and effectiveness of healthcare delivery, healthcare providers must embrace technological change. Investing in modern EHR solutions and leveraging innovative technologies can help streamline workflows, enhance data accuracy, and optimize revenue cycle management processes.

Benefits of Technological Change
- Streamlined Workflows: Modern EHR systems offer intuitive interfaces and automated workflows, reducing administrative burden and improving productivity.
- Improved Data Accuracy: Electronic health records minimize errors associated with manual data entry and paper-based documentation, ensuring the integrity and reliability of patient information.
- Enhanced Revenue Cycle Management: Advanced features such as automated billing, claims processing, and revenue analytics help optimize revenue cycle performance and maximize revenue capture.
Overcoming Resistance to Innovation
Despite the potential benefits, the adoption of new technologies in healthcare often faces resistance from stakeholders who are accustomed to traditional practices. Overcoming resistance to innovation requires effective change management strategies, communication, and support from leadership.
Strategies for Overcoming Resistance
- Education and Training: Providing comprehensive training programs and resources to familiarize healthcare professionals with the benefits and functionalities of new technologies.
- Engaging Stakeholders: Involving frontline staff in the decision-making process and soliciting their feedback and input on the implementation of new EHR solutions.
- Demonstrating Value: Highlighting the positive impact of technological innovations on patient care outcomes, operational efficiency, and financial performance.
Harnessing the Power of Modern EHR Solutions
Modern EHR solutions offer a wide range of features and functionalities designed to address the evolving needs of healthcare organizations and improve the delivery of patient care. From cloud-based platforms to mobile applications, these solutions empower providers to deliver more personalized and efficient healthcare services.
Key Features of Modern EHR Solutions
- Cloud-Based Architecture: Cloud-based EHR systems offer scalability, flexibility, and accessibility, allowing providers to access patient information securely from any location or device.
- Interoperability Standards: Modern EHR solutions adhere to interoperability standards such as HL7 and FHIR, enabling seamless data exchange and communication between different systems and healthcare providers.
- Clinical Decision Support: Built-in clinical decision support tools provide real-time guidance and recommendations to healthcare professionals, enhancing diagnostic accuracy and treatment outcomes.
Strategies for Effective Implementation
Successful implementation of modern EHR solutions requires careful planning, collaboration, and support from all stakeholders involved. Healthcare organizations must develop a comprehensive implementation strategy that addresses technical, operational, and cultural factors.
Steps for Effective Implementation
- Needs Assessment: Conducting a thorough assessment of organizational needs, workflows, and goals to identify the most suitable EHR solution.
- Change Management: Developing a change management plan that outlines roles, responsibilities, and communication strategies to facilitate a smooth transition to the new system.
- Training and Support: Providing ongoing training and support to users to ensure they are proficient in using the new EHR system effectively.
Addressing Privacy and Security Concerns
Privacy and security are paramount in healthcare, and the adoption of EHR systems introduces new challenges and risks in safeguarding patient information. Healthcare organizations must implement robust security measures and protocols to protect sensitive data from unauthorized access and breaches.
Strategies for Ensuring Privacy and Security
- Data Encryption: Encrypting patient data both at rest and in transit to prevent unauthorized access and ensure confidentiality.
- Access Controls: Implementing role-based access controls to restrict access to patient information based on users’ roles and responsibilities.
- Regular Audits and Monitoring: Conducting regular audits and monitoring of EHR systems to detect and mitigate security vulnerabilities and breaches.
Embracing Interoperability for Seamless Integration
Interoperability is essential for enabling seamless data exchange and communication between different EHR systems and healthcare providers. By adopting interoperability standards and leveraging integration tools, healthcare organizations can improve care coordination, reduce duplicative testing, and enhance patient outcomes.

Benefits of Interoperability
- Improved Care Coordination: Interoperable EHR systems allow healthcare providers to access and share patient information efficiently, facilitating better care coordination and collaboration.
- Reduced Administrative Burden: Seamless integration between EHR systems and other healthcare applications streamlines administrative processes, reducing duplication of data entry and paperwork.
- Enhanced Patient Engagement: Interoperability enables patients to access their health records and communicate with healthcare providers more easily, empowering them to take an active role in their healthcare management.
The Role of Patient Engagement
Patient engagement is essential for improving health outcomes and reducing healthcare costs. By actively involving patients in their care and providing them with the tools and resources they need to make informed decisions, healthcare organizations can promote better health outcomes and satisfaction.
Strategies for Enhancing Patient Engagement
- Patient Portals: Providing patients with secure online portals where they can access their health records, schedule appointments, and communicate with their healthcare providers.
- Health Education: Offering educational resources and materials to help patients understand their conditions, treatment options, and preventive measures.
- Remote Monitoring: Leveraging remote monitoring technologies to track patients’ health status and provide timely interventions and support.
Conclusion
In conclusion, the EHR crisis presents significant challenges for healthcare organizations, impacting both financial performance and the quality of patient care. However, by embracing technological change, implementing modern EHR solutions, and fostering a culture of innovation, healthcare providers can overcome these challenges and deliver better, more efficient care to their patients.